MAT Pregnancy: What You Need to Know About Medication-Assisted Treatment During Pregnancy
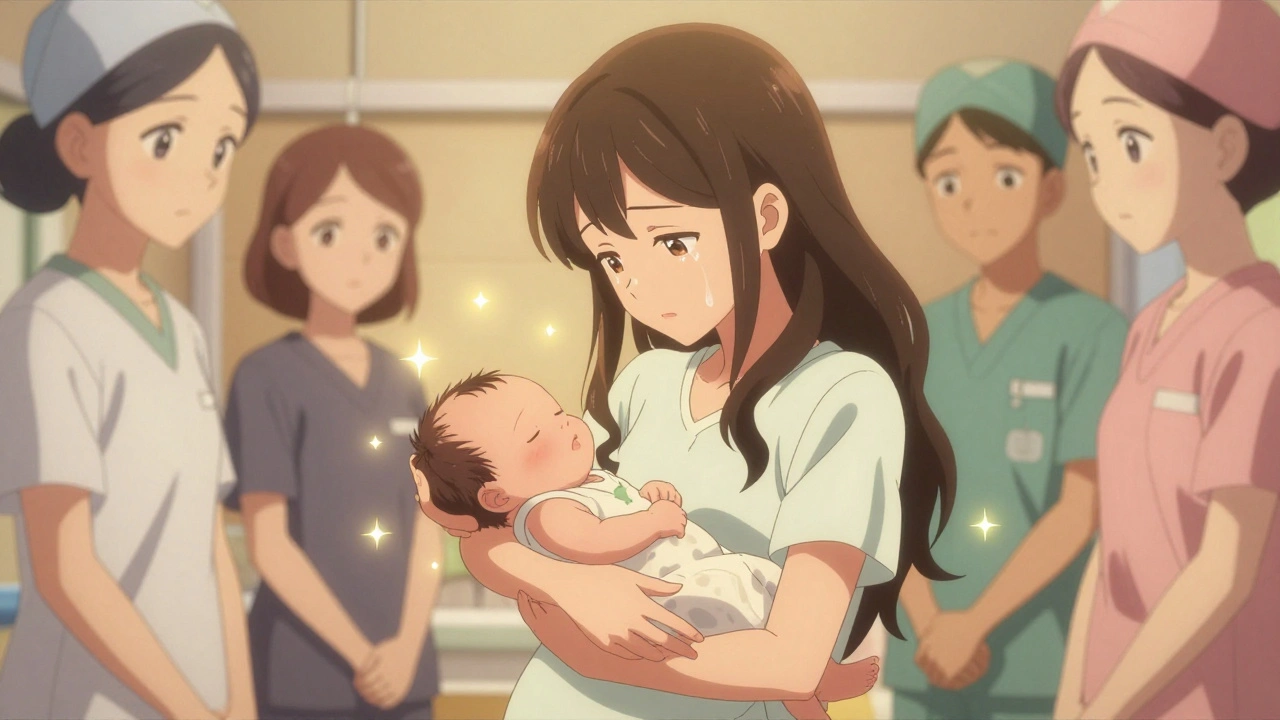
When someone is pregnant and struggling with opioid use disorder, a chronic condition where a person continues using opioids despite harmful consequences. Also known as substance use disorder, it affects thousands of pregnant women each year. Medication-assisted treatment, a proven approach combining FDA-approved medications with counseling and behavioral therapy. Also known as MAT, it’s the gold standard for managing addiction during pregnancy—not just for the mother’s health, but for the baby’s too. Unlike quitting cold turkey, which can trigger miscarriage, preterm labor, or fetal distress, MAT stabilizes the body, reduces cravings, and lowers the risk of relapse. This isn’t replacing one drug with another—it’s giving the body what it needs to heal while protecting a growing life.
The most common medications used in MAT pregnancy, the use of approved drugs like methadone or buprenorphine to treat opioid dependence during gestation are methadone and buprenorphine. Both cross the placenta, but they do so in a controlled way that prevents the highs and crashes of street opioids. Studies show babies born to mothers on MAT have fewer complications than those born to mothers who use heroin or fentanyl. They’re more likely to be born at a healthy weight, stay in the womb longer, and need less intensive care after birth. Even better, MAT lets mothers stay engaged in prenatal care, therapy, and support systems—all critical for long-term recovery.
It’s not just about the drugs. prenatal medication safety, the practice of evaluating and managing drug use during pregnancy to minimize harm to the fetus means knowing what’s safe, what’s risky, and what to avoid. For example, lisinopril-HCTZ and other ACE inhibitors are dangerous during pregnancy—they can cause kidney damage and even fetal death. But that’s not the only concern. Some antidepressants, pain meds, and even over-the-counter supplements can interfere with fetal development. That’s why MAT programs don’t just hand out pills—they coordinate with OB-GYNs, pharmacists, and mental health providers to build a full safety net around the mother and baby.
What you’ll find in the posts below isn’t just theory—it’s real, actionable info from people who’ve been there. You’ll see how to report unsafe prescriptions, why switching meds during pregnancy needs careful planning, how to track drug interactions, and what to do if you’re on a medication that’s not safe for pregnancy. These aren’t abstract guidelines. They’re step-by-step tools for protecting yourself and your baby when the stakes couldn’t be higher.
Opioids During Pregnancy: Risks, Withdrawal, and What You Need to Know
Opioids during pregnancy require careful medical management. Learn the risks of withdrawal, how medication-assisted treatment helps, what to expect after birth, and why stigma shouldn't stand in the way of care.
December 1 2025