When older adults switch from brand-name drugs to generics, it’s not just a cost-saving move-it’s a decision that can affect how they feel, function, and even if they end up back in the hospital. Many seniors are told generics are just as good, and in most cases, they are. But for someone taking five, six, or more pills a day-many of them for chronic conditions like high blood pressure, thyroid disease, or heart rhythm problems-the switch isn’t always simple. And it’s not just about price. It’s about how their bodies change with age, what they believe about their meds, and whether anyone took the time to explain what’s really going on.
Why Generics Are Often the Right Choice
Generic drugs aren’t cheap knockoffs. They’re required by the FDA to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. That means if you’re taking a generic version of lisinopril for high blood pressure, you’re getting the exact same chemical as the brand-name Zestril. The only differences? The color, shape, or filler ingredients-and the price. On average, seniors save about $327 a year per medication when switching to generics, according to AARP’s 2023 analysis. Across Medicare Part D, 89.2% of all prescriptions filled in 2022 were generics. That’s over half a billion prescriptions. For many, it’s the only way they can afford their treatment.But Age Changes How Drugs Work
Your body doesn’t process medicine the same way at 80 as it did at 40. Kidneys slow down. Liver blood flow drops. Body fat increases while muscle mass declines. All of this changes how drugs are absorbed, distributed, and cleared from the body. For most medications, these changes don’t make generics unsafe. But for drugs with a narrow therapeutic index-where the difference between a helpful dose and a dangerous one is tiny-small differences in how a generic is made can matter. Take warfarin, for example. It’s used to prevent blood clots, but if your blood gets too thin, you risk bleeding. Too thick, and you risk a stroke. A 2021 study of nearly 135,000 patients found that switching from brand-name Coumadin to a generic version led to an 18.3% higher chance of ending up in the emergency room within 30 days. That’s why the American Geriatrics Society says: don’t automatically swap warfarin without close monitoring. INR levels need to be checked more often after the switch. The same caution applies to levothyroxine, the thyroid hormone replacement. Some seniors report feeling worse after switching from Synthroid to a generic version. On Reddit’s r/geriatrics, 73% of 147 commenters said their fatigue, brain fog, or weight gain returned after the switch. While large studies haven’t proven generics are less effective, the fact that so many older patients report changes suggests that for some, the switch triggers real symptoms-even if it’s not a pharmacological difference, it could be a psychological one, or a subtle variation in absorption.Polypharmacy Makes Everything Riskier
About 46% of Medicare beneficiaries take five or more medications daily. That’s called polypharmacy. And it’s the biggest risk factor for bad reactions. With so many drugs in the system, even tiny changes in how one pill is absorbed can throw off the whole balance. A 2024 JAMA Network Open review found that seniors on five or more drugs are twice as likely to have a dangerous drug interaction. And it’s not just prescription meds. Over-the-counter drugs are a hidden danger. One in four seniors take multiple OTC painkillers, sleep aids, or antihistamines without realizing they’re doubling up. For example, 45% of acetaminophen use in older adults comes from multi-ingredient products-like cold medicines-that can push them past the safe daily limit of 3,000 mg, risking liver damage. The same goes for diphenhydramine (Benadryl), which can cause confusion, dizziness, and falls in older people. The Beers Criteria and STOPP/START guidelines, used by doctors and pharmacists to spot risky prescriptions, list over 50 medications that should be avoided or used with extreme caution in seniors. These include certain anticholinergics, benzodiazepines, and NSAIDs like ibuprofen, which can cause kidney failure or stomach bleeding in older adults. Switching to generics doesn’t fix these problems-it just makes them cheaper.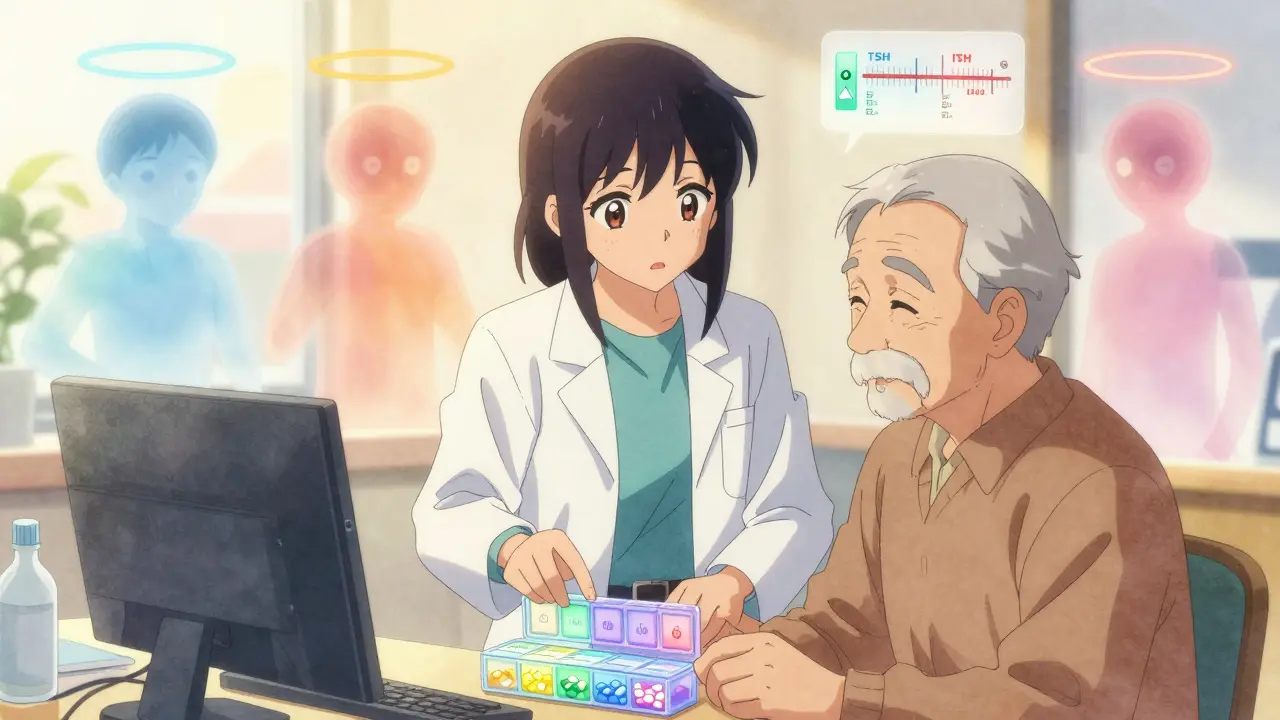
Perception Matters More Than You Think
A 2023 study of 315 older adults in New York found that fewer than half believed generics were as safe or effective as brand-name drugs. That’s not because they’re wrong-it’s because they’ve been told stories. Maybe a neighbor’s cousin had a bad reaction. Maybe the pill looks different. Maybe the pharmacist didn’t explain why the change happened. In low-income, racially diverse senior populations, one in four believe generics are less effective. One in five think they’re less safe. And 20-40% are just unsure. These beliefs aren’t just opinions-they affect behavior. If you don’t trust your medication, you’re less likely to take it regularly. And that’s when things go wrong. Non-adherence rates among elderly patients range from 21% to 55%. That’s not because they’re forgetful. It’s because they’re afraid.What Doctors and Pharmacists Should Do
Switching seniors to generics shouldn’t be automatic. It should be intentional. And it should come with support. First, use the teach-back method. Ask the patient: “Can you tell me in your own words why we’re switching to this pill?” Studies show this simple technique improves adherence by 42%. Don’t just hand them a new bottle. Show them the old pill and the new one side by side. Say: “This is the same medicine, just made by a different company. The color changed because the filler is different, but the active part is identical.” Second, involve a clinical pharmacist. A 2024 meta-analysis found that when pharmacists joined the care team, they reduced inappropriate prescriptions by 37.2%. They’re trained to spot dangerous combinations, check for duplications, and flag high-risk switches. They can also help patients understand their meds without jargon. Third, use technology. Computerized systems that alert doctors when a senior is about to get a new high-risk drug or a generic switch can improve prescribing accuracy by nearly 30%. These tools don’t replace human judgment-they support it.When to Be Cautious
Not all generics are equal when it comes to older adults. Be extra careful with:- Warfarin - Monitor INR closely for 4-6 weeks after switching.
- Levothyroxine - Stick with one brand or generic consistently. Don’t switch back and forth.
- Seizure medications - Phenytoin, carbamazepine, and valproate have narrow windows. Changes can trigger seizures.
- Immune suppressants - Cyclosporine and tacrolimus used after transplants require tight monitoring.
- Heart rhythm drugs - Amiodarone and digoxin can be dangerous if levels shift.

What Seniors Can Do
If you’re an older adult on multiple meds:- Keep a written list of every pill you take-including vitamins, supplements, and OTC drugs.
- Ask your pharmacist: “Is this the same as what I was taking before?”
- Don’t assume a new pill is a mistake. Ask why the change happened.
- If you feel different after a switch-fatigue, dizziness, confusion, heart palpitations-tell your doctor right away. Don’t wait.
- Use a pill organizer. It helps you notice if you’re missing doses or taking the wrong one.
The Bigger Picture
By 2030, nearly 94% of Medicare prescriptions will be generic. That’s good for the system. But if we don’t fix how we communicate with seniors about these changes, we’ll just be saving money while increasing hospital visits. The goal isn’t just to switch pills-it’s to keep people safe, healthy, and confident in their care. The science says generics work. But the human side? That’s where the real work begins.Are generic medications really as effective as brand-name drugs for elderly patients?
Yes, for most medications, generics are just as effective. They must meet strict FDA standards to prove they deliver the same amount of active ingredient into the bloodstream as the brand-name version. But for drugs with a narrow therapeutic index-like warfarin, levothyroxine, or seizure medications-small differences in how the body absorbs the drug can matter. These cases require closer monitoring after a switch. For the majority of seniors taking blood pressure or cholesterol meds, there’s no meaningful difference in outcomes.
Why do some older adults feel worse after switching to generics?
Some seniors report symptoms like fatigue, brain fog, or heart palpitations after switching, especially with thyroid or heart medications. This isn’t always due to pharmacological differences. The change in pill size, color, or taste can trigger psychological responses. In others, it may be due to unmonitored shifts in drug absorption caused by age-related changes in digestion or kidney function. If symptoms appear after a switch, it’s important to report them to your doctor and get blood tests done-not to assume the generic is bad, but to make sure your dose is still right.
Can switching to generics cause dangerous drug interactions?
Switching to a generic drug doesn’t cause interactions-it’s the number of drugs you’re taking that does. Seniors on five or more medications are at much higher risk. The real danger comes when a new generic is added without reviewing the full list. For example, a new generic blood pressure pill might interact with an OTC painkiller or supplement you’ve been taking. That’s why a pharmacist review is so important. Always bring your full list of meds to every appointment.
Should seniors avoid all generics because of the risks?
No. Most seniors benefit from generics. They save hundreds of dollars a year and help ensure people can afford their meds. The key is not to avoid them-but to manage the switch carefully. For high-risk drugs like warfarin or levothyroxine, work with your doctor to monitor your response. For common meds like statins or metformin, generics are safe and effective. The goal is smart switching, not avoiding generics altogether.
How can I tell if my generic medication is working the same way?
Pay attention to how you feel. If you’ve been stable on your medication and suddenly feel worse-more tired, dizzy, confused, or short of breath-it could be a sign. Also, ask your doctor for lab tests. For example, if you’re on warfarin, check your INR. If you’re on thyroid medication, get your TSH level tested. These numbers tell you if your body is responding the same way. Don’t rely on how the pill looks. Trust the numbers.
What should I do if my pharmacy switches my generic without telling me?
You have the right to ask for the brand or a specific generic. In many states, pharmacists are required to notify you before switching. If they don’t, call your doctor or pharmacy and say: “I was on X brand, and now I’m getting a different pill. Can you confirm this is the same?” If you’re concerned, ask for a 30-day supply of your old version while you discuss it with your provider. Never stop taking your medication without talking to someone first.
Are there financial assistance programs for seniors who can’t afford brand-name drugs?
Yes. Many drug manufacturers offer patient assistance programs that provide brand-name or generic medications at low or no cost to seniors with limited income. Medicare Part D also has a coverage gap (donut hole) relief program. Check with your pharmacy, visit the Medicare website, or call 1-800-MEDICARE. You don’t have to choose between your health and your budget.

Alexandra Enns
January 23, 2026 AT 13:57This whole article is a corporate shill for Big Pharma’s generic racket. You think the FDA’s ‘same active ingredient’ crap means anything? I’ve seen seniors on warfarin go from stable INRs to ER trips after switching - and no, it’s not ‘just psychology.’ The fillers are loaded with cornstarch and talc that mess with absorption. And don’t get me started on how Indian manufacturers cut corners. This isn’t medicine - it’s a cost-cutting lottery.
Marie-Pier D.
January 24, 2026 AT 04:42Thank you for writing this with so much heart 💙 I’ve seen my 82-year-old mom cry because her thyroid pill changed color and she thought she was being poisoned. It’s not about the science - it’s about trust. The fact that we don’t sit down with seniors, show them the old pill and the new one, and say ‘this is the same medicine, just in a different jacket’… that’s the real failure. Please, pharmacists - don’t just swap. Explain.
lorraine england
January 25, 2026 AT 21:05Let’s be real - most of these ‘I felt worse after switching’ stories are just people being hypochondriacs. If your TSH was stable before and now it’s stable again, you’re fine. The placebo effect is real, folks. Also, if you’re taking 6+ meds, maybe the problem isn’t the generic - it’s that you’re on way too many pills. Stop blaming the pharmacy and start asking your doctor to deprescribe.
Kevin Waters
January 25, 2026 AT 21:29Great breakdown. I’m a clinical pharmacist and I can tell you - the biggest issue isn’t the generics themselves, it’s the lack of follow-up. I’ve had patients come in saying, ‘I switched and now I’m dizzy’ - and we find they’re taking three different OTC sleep aids with diphenhydramine. The generic switch was just the trigger. We need more pharmacist-led med reviews, especially at discharge. It’s not rocket science - just basic care.
Kat Peterson
January 26, 2026 AT 16:27OMG I JUST HAD THIS HAPPEN TO MY GRANDMA 😭 She went from Synthroid to some generic and started forgetting her own name. I called the pharmacy - they said ‘it’s the same thing.’ SAME THING?! The pill is a different shade of white and now she’s crying at dinner because she thinks she’s turning into a zombie. This is a medical horror story. Someone needs to sue someone. 🤮
Helen Leite
January 27, 2026 AT 19:50THEY’RE HIDING THE TRUTH. The FDA doesn’t test generics on old people. They test them on 25-year-old college kids. And the companies? They use cheap fillers that cause inflammation. That’s why seniors are getting dementia faster now. It’s not age - it’s the poison in the pills. I’ve got a spreadsheet of 87 cases. The government is covering it up. You think your ‘generic’ is safe? Check the manufacturer. If it’s not from the US or Germany - don’t take it. 🚨
venkatesh karumanchi
January 29, 2026 AT 19:50My uncle switched to generic metformin and his blood sugar went wild. He didn’t tell anyone for weeks because he didn’t want to be a bother. Finally, he went to the clinic and they found his levels were off by 40%. He got switched back. Point is - don’t assume. Test. Watch. Listen to your body. And if you’re scared, ask. No one will think you’re silly for caring about your health.
Sharon Biggins
January 31, 2026 AT 04:45so i just wanted to say thank you for this post. my mom is 78 and she was so scared when her blood pressure med changed color. i sat with her and showed her the old and new pill side by side and said ‘this is the same medicine, just a different company made it’. she cried. but then she smiled. we got her INR checked and it was fine. small things matter. thank you for reminding us.
John McGuirk
February 1, 2026 AT 11:32Generics? More like generic lies. I’ve been watching this for years. The FDA lets these companies get away with 5% variation in absorption - but for a 75-year-old with kidney issues, that 5% is a death sentence. And the pharmacy chains? They don’t care. They get paid per pill. They don’t care if you end up in the ICU. This is profit-driven healthcare at its worst. Wake up people.
siva lingam
February 1, 2026 AT 23:26