When your kidneys are damaged, high blood pressure doesn’t just worsen your heart-it accelerates kidney failure. For millions with chronic kidney disease (CKD), controlling blood pressure isn’t just about feeling better. It’s about stopping the clock on kidney damage. And two classes of drugs-ACE inhibitors and ARBs-have become the cornerstone of this fight.
Why Blood Pressure Matters in Kidney Disease
Your kidneys filter waste and extra fluid from your blood. When they’re healthy, they handle pressure well. But when damage sets in-whether from diabetes, high blood pressure, or other causes-the tiny filters inside your kidneys (glomeruli) start to leak. Protein spills into your urine. Fluid builds up. Pressure rises inside the kidneys. This creates a vicious cycle: high pressure damages more filters, which makes the pressure worse.
Studies show that keeping systolic blood pressure below 130 mmHg can slow kidney decline by up to 40% in people with proteinuria. But not all blood pressure meds do this equally. ACE inhibitors and ARBs are unique because they don’t just lower pressure-they directly protect the kidney’s filtering units.
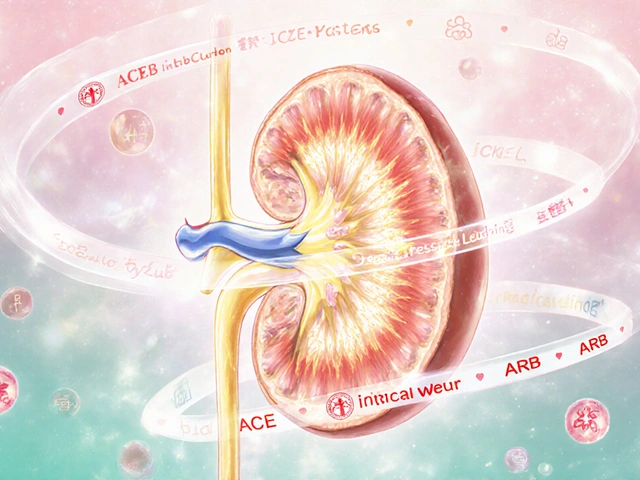
How ACE Inhibitors and ARBs Work
Both drugs target the same system: the renin-angiotensin-aldosterone system, or RAAS. This system controls blood pressure by tightening blood vessels and making your body hold onto salt and water. In kidney disease, RAAS goes into overdrive, squeezing the kidneys harder than they can handle.
ACE inhibitors (like lisinopril, enalapril, benazepril) block the enzyme that turns angiotensin I into angiotensin II-the main hormone that constricts blood vessels. Less angiotensin II means relaxed vessels, lower pressure, and less strain on the kidneys.
ARBs (like losartan, valsartan, irbesartan) work differently. They don’t stop angiotensin II from being made. Instead, they block its receptors so it can’t bind and cause damage. The result? Similar blood pressure lowering, similar protection.
Both reduce intraglomerular pressure-the pressure inside the kidney’s filters. This is key. Lower pressure = less protein leaking out = slower kidney damage. Clinical trials show these drugs cut proteinuria by 30-50%. That’s not just a lab number. It’s a sign your kidneys are holding on.
Proven Benefits: Slowing Kidney Failure
It’s not theory. It’s data.
A 2024 study of 1,237 patients with advanced CKD (eGFR under 20) found those taking ACE inhibitors or ARBs had a 34% lower risk of needing dialysis or a transplant over 34 months. Another trial in the UK followed patients with stage IV or V CKD for three years. Those who kept taking their ACE inhibitor or ARB had better kidney function than those who stopped-even though their kidneys were already severely damaged.
Meta-analyses confirm: compared to other blood pressure meds, ACE inhibitors and ARBs reduce the risk of end-stage kidney disease by 25%. In people with diabetes and kidney disease, the benefit is even stronger. These drugs aren’t just helpers-they’re the most effective tools we have to delay kidney failure.
ACE Inhibitors vs. ARBs: What’s the Difference?
Both work similarly. But they don’t feel the same.
ACE inhibitors are older and cheaper. Lisinopril is one of the most prescribed drugs in the U.S., with over 127 million prescriptions in 2023. But about 1 in 5 people develop a dry, nagging cough. It’s not dangerous, but it’s annoying enough that many stop taking it.
There’s also a rare but serious risk: angioedema. Swelling in the face, lips, or throat. It happens in less than 1 in 500 people, but it’s an emergency if it does.
ARBs were developed to avoid these side effects. They rarely cause cough. Angioedema risk is even lower. For people who can’t tolerate ACE inhibitors, ARBs are the clear next step. Valsartan and losartan are among the top-selling ARBs.
When it comes to lowering blood pressure and reducing proteinuria, they’re nearly identical. The choice often comes down to side effects, cost, and patient preference.

When to Use Them-And When to Be Careful
Guidelines from the American College of Cardiology and Kidney Disease: Improving Global Outcomes (KDIGO) say: if you have CKD and protein in your urine, start an ACE inhibitor or ARB. That’s true even if your blood pressure is normal.
But there are red flags:
- High potassium: These drugs can raise potassium levels. If your blood potassium goes above 5.0 mmol/L, your doctor may adjust your dose or diet.
- Drop in kidney function: After starting, your eGFR might dip by 10-30%. That’s normal if it stabilizes. But if it drops more than 30% from baseline, or if you’re dehydrated, it could mean trouble.
- Advanced CKD: Many doctors still avoid these drugs in stage 4 or 5 CKD. But new data says: don’t stop them. A 2024 study showed patients with eGFR as low as 19.8 still benefited. Stopping them didn’t protect kidneys-it hurt them.
Doctors are now encouraged to keep these drugs going as long as potassium stays under 5.5 mmol/L and eGFR doesn’t crash. Monthly blood tests in the first few weeks are standard. After that, every 3-6 months.
Why So Many People Aren’t Getting Them
Here’s the shocking part: only about 58% of patients with advanced CKD are on an ACE inhibitor or ARB. In early-stage CKD, that number jumps to 82%. Why the gap?
Fear. Misinformation. Outdated thinking.
Some doctors worry about hyperkalemia or sudden kidney decline. But the data shows: the risk of harm from stopping these drugs is higher than the risk from using them. A 2023 review by Dr. Rajiv Agarwal put it bluntly: “Fear of adverse events has led to therapeutic nihilism in advanced CKD, denying patients proven benefits without evidence of harm.”
Patients, too, stop on their own. A National Kidney Foundation survey found 28% quit because of cough. 12% stopped because high potassium meant giving up bananas, potatoes, and oranges. But with proper monitoring and diet tweaks, most side effects are manageable.
What About Combining ACE Inhibitors and ARBs?
It sounds logical: block the system at two points. More protection, right?
Early studies showed combo therapy cut proteinuria by an extra 15-20%. But the Veterans Affairs Nephropathy Trial found it doubled the risk of acute kidney injury and increased hyperkalemia by 50%. No improvement in long-term kidney or heart outcomes. Just more hospital visits.
Today, guidelines strongly advise against combining ACE inhibitors and ARBs. The risks outweigh the benefits. Stick with one. Maximize the dose. Add other blood pressure meds if needed-diuretics, calcium channel blockers, or others.

What’s Next? Newer Drugs on the Horizon
Science doesn’t stop. The 2024 PARADIGM-HF trial extension looked at sacubitril/valsartan-a new class called ARNIs (angiotensin receptor-neprilysin inhibitors). Used in heart failure patients with CKD, this combo reduced kidney function decline by 22% compared to enalapril.
It’s not yet approved for kidney disease alone. But it hints at the future: drugs that don’t just block RAAS, but also boost protective hormones. For now, ACE inhibitors and ARBs remain the gold standard.
Real Stories, Real Outcomes
On Reddit, a 58-year-old with stage 4 CKD wrote: “I’ve been on lisinopril for 5 years. My proteinuria dropped from 800 mg/day to 150. My eGFR held steady at 22. I check potassium every 3 months. I’m not on dialysis. This drug saved my kidneys.”
Another user, on the same thread, said: “I stopped my ARB because my doctor said it was too risky. Six months later, my eGFR dropped 30%. I had to restart. Don’t quit without a plan.”
These aren’t anecdotes. They’re echoes of clinical data. The right drug, monitored properly, changes outcomes.
What You Should Do
If you have kidney disease:
- Ask your doctor if you have protein in your urine. If yes, you’re a candidate for an ACE inhibitor or ARB-even if your blood pressure is normal.
- If you’re already on one, don’t stop unless your doctor tells you to. A small dip in eGFR isn’t a reason to quit.
- Get blood tests 1-2 weeks after starting or changing dose. Check potassium and eGFR.
- If you get a cough on an ACE inhibitor, don’t suffer. Switch to an ARB. It’s safe and just as effective.
- Don’t fear potassium. Work with a dietitian. You don’t have to eliminate potassium-just manage it.
These drugs aren’t magic. But they’re the closest thing we have to a time machine for your kidneys. Use them right, and you buy yourself years.
Can ACE inhibitors or ARBs reverse kidney damage?
No, they can’t reverse existing damage. But they can slow or stop further damage. Studies show they reduce the rate of kidney function decline by 20-40%. That means delaying dialysis by years-even in advanced disease. The goal isn’t to fix broken filters, but to protect the ones still working.
Are ACE inhibitors and ARBs safe for people with diabetes?
Yes, they’re actually preferred. Diabetic kidney disease is one of the strongest reasons to use them. The landmark DCCT and UKPDS trials showed ACE inhibitors and ARBs cut the risk of kidney failure in type 1 and type 2 diabetes by up to 30%. They’re a standard part of diabetes care when proteinuria is present.
What if my potassium is high? Do I have to stop the medication?
Not always. If potassium is between 5.0 and 5.5 mmol/L, your doctor may lower the dose, adjust your diet, or add a potassium binder like patiromer. Stopping the drug entirely is usually unnecessary. In fact, stopping can make kidney function worse. The key is monitoring-not avoidance.
Can I take ACE inhibitors or ARBs if I’m on dialysis?
Yes, many patients on dialysis still take them. They help control blood pressure, reduce heart strain, and lower the risk of hospitalization. Potassium levels are monitored closely because dialysis can cause swings. But these drugs are not automatically stopped once dialysis starts. The decision is individualized.
Do I need to take these drugs for life?
Usually, yes. Kidney disease is progressive, and the protective effect lasts as long as you take the medication. Stopping increases the risk of rapid decline. If you’re doing well with no side effects and stable labs, continuing is the standard of care. Always consult your doctor before making changes.
Final Thoughts
For people with kidney disease, ACE inhibitors and ARBs aren’t optional. They’re essential. The evidence is clear, the guidelines are consistent, and the stakes are high. The fear of side effects shouldn’t override the benefit of protection. With smart monitoring, these drugs are safer than ever. And for many, they’re the difference between managing kidney disease-and living with it.

Ryan Everhart
November 14, 2025 AT 00:24So basically these drugs are the only thing keeping half the diabetic population off dialysis and yet doctors still act like they’re giving out heroin? Wild.
David Barry
November 15, 2025 AT 13:08Let’s cut through the noise. ACEi/ARBs reduce intraglomerular pressure via efferent arteriolar vasodilation - that’s the mechanistic gold. Proteinuria reduction isn’t a side effect, it’s the primary therapeutic endpoint. Any clinician who stops these in stage 4 CKD because of a 15% eGFR dip is practicing fear-based medicine, not evidence-based care. The 2024 meta-analysis in JASN is unambiguous: mortality increases when you withdraw. Period.
Alyssa Lopez
November 16, 2025 AT 18:44Okay but like… why are we even talking about this? Like, if you got CKD you’re already a goner, right? Like, why waste money on drugs when you’re gonna need dialysis anyway? Also, potassium is bad, I heard it kills you. Bananas = death. I’m not taking no pills that make me eat salad.
edgar popa
November 17, 2025 AT 19:59My dad’s been on lisinopril for 7 years. His kidneys are still working. He eats bananas. He checks his numbers. He’s alive. Don’t overthink it. Take the pill. Talk to your doc. You got this.
Shante Ajadeen
November 19, 2025 AT 09:36I’m so glad this was written so clearly. I was scared to start mine because of the cough thing, but switching to losartan was easy. My doc said it’s like swapping one comfy chair for another - same support, no squeak. You’re not alone in this.
dace yates
November 20, 2025 AT 02:55Does anyone know if ARBs are harder to get on Medicaid? My pharmacy said valsartan costs $45 without insurance, but lisinopril is $4. Is that normal or am I being screwed?
Danae Miley
November 21, 2025 AT 01:10David Barry’s comment above is correct, but it lacks context: the 30% eGFR drop threshold is not a universal rule. It’s baseline-dependent. A patient with eGFR 60 dropping to 42 is fine. A patient with eGFR 25 dropping to 17 requires reevaluation. Always interpret changes relative to starting values, not absolute numbers. This is basic nephrology - yet still overlooked.
Charles Lewis
November 22, 2025 AT 06:49It is worth noting, with considerable emphasis, that the renin-angiotensin-aldosterone system, or RAAS, represents one of the most extensively studied physiological pathways in modern nephrology. The pharmacological modulation of this system via either angiotensin-converting enzyme inhibition or angiotensin receptor blockade has been validated across multiple large-scale, multicenter, randomized controlled trials spanning more than three decades. The consistency of outcomes - reduced proteinuria, slowed progression of glomerulosclerosis, and delayed time to end-stage renal disease - is not merely statistically significant; it is clinically profound. To withhold these agents in the presence of proteinuric kidney disease, regardless of baseline blood pressure, constitutes a deviation from established standard of care, and may, in some instances, be considered negligent under current medical ethics frameworks.
Samantha Wade
November 23, 2025 AT 22:50Stop letting fear dictate your health. If you’re on dialysis and still on an ARB, that’s not a mistake - that’s strategy. Potassium can be managed. Kidney function dips are temporary. The real danger is stopping. I’ve seen patients recover function after restarting - because they listened to the data, not the noise. You deserve to live longer. Take the pill. Get the labs. Talk to your team. You’re not alone.
Renee Ruth
November 24, 2025 AT 04:52They’re lying to you. I know. I was on lisinopril. They said it was ‘protecting’ me. Then my potassium hit 6.1. I almost died in the ER. They didn’t tell me the truth: these drugs are a trap. They make you feel like you’re doing something, but really? You’re just waiting for your body to fail slower. And now I’m on dialysis. So yeah - maybe don’t take them. I’m not saying that. I’m just saying… I’m here. And I’m not the only one.