When you’re first told you have localized cancer, the word "treatment" can feel overwhelming. You hear terms like radiation and surgery, and suddenly you’re expected to choose between two major medical paths-both aimed at stopping the cancer in its tracks. But here’s the truth: neither is universally better. The right choice depends on your cancer type, your body, your life, and what matters most to you.
What Does "Local Control" Even Mean?
Local control means stopping cancer from growing or spreading in one specific area-like your prostate, lung, or breast-without going after cancer that may have already moved elsewhere. This isn’t about curing advanced disease. It’s about removing or destroying the tumor where it started. For many people with early-stage cancer, this is the most important step.Two main tools do this: surgery, which cuts it out, and radiation, which zaps it with high-energy beams. Both can be curative. But they work in very different ways-and come with very different trade-offs.
Surgery: Removing the Problem
Surgery means physically taking the tumor out. For prostate cancer, that’s a radical prostatectomy. For lung cancer, it could be a lobectomy-removing one of the five lobes of the lung. The goal? Get it all. Remove the cancer, get a clear margin, and know exactly what you’re dealing with.The big advantage? Immediate results. After surgery, the tumor is gone. Pathologists examine it under a microscope and give you a detailed report: stage, grade, margins. That info guides everything else-whether you need more treatment, and what kind.
But it’s not simple. A prostatectomy usually takes 2-4 hours. You’ll be in the hospital for 1-3 days. Recovery? You’re looking at 4-6 weeks before you feel like yourself again. And the side effects? They’re real. About 14% of men with low-risk prostate cancer still have urinary leakage 10 years later. For high-risk cases, that number jumps to 25%. Erectile dysfunction hits 40-60% of men after surgery, depending on nerve-sparing techniques and age.
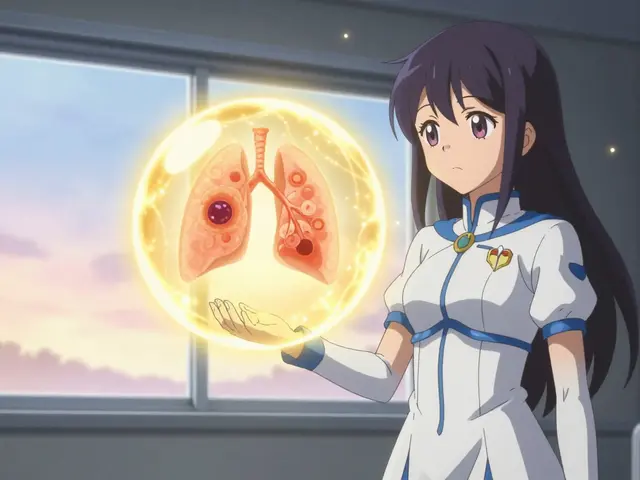
For lung cancer, surgery is even more demanding. A VATS or robotic lobectomy requires 3-7 days in the hospital. Full recovery can take 6-8 weeks. You’re not just healing from an incision-you’re rebuilding lung capacity. Breathing will feel different. Walking up stairs? Harder at first.
Radiation: Zapping It Without Cutting
Radiation therapy doesn’t remove the tumor. It kills cancer cells with targeted beams of energy. Modern machines can hit a tumor with 1-2 millimeter precision, sparing healthy tissue better than ever.For prostate cancer, traditional radiation means daily 15-30 minute sessions, 5 days a week, for 7-9 weeks. That’s a lot of trips. If you live far from a treatment center, it can mean weekly travel, time off work, and disrupted routines. But newer methods like SBRT (stereotactic body radiation therapy) shrink that to just 1-5 sessions over 1-2 weeks. No hospital stay. You walk in, get treated, walk out.
For early-stage lung cancer, SBRT is now a standard option-even for people who can’t have surgery. A 2022 study of over 30,000 patients found that surgery gave a 71.4% five-year survival rate, while SBRT gave 55.9%. But here’s the catch: the SBRT group included patients who weren’t healthy enough for surgery. When you compare only those who could have had either option, the survival gap narrows significantly.
Side effects? Different, but no less real. Radiation doesn’t cause urinary leakage like surgery does. But it can damage nearby tissues over time. About 8% of men who get radiation for prostate cancer develop serious bowel problems-rectal bleeding, urgency, incontinence-within 10 years. That’s double the rate of surgical patients. And for lung cancer, radiation can cause fatigue, skin irritation, and sometimes long-term lung scarring.
Prostate Cancer: The Data Doesn’t Give a Clear Winner
The biggest debate happens in prostate cancer. Two major studies tell different stories.The ProtecT trial, published in 2016, followed 1,643 men with low- to intermediate-risk prostate cancer. Ten years later, survival rates were nearly identical: 96.8% for surgery, 95.7% for radiation. But surgery had slightly lower rates of cancer coming back. Radiation? Higher chance of needing more treatment later.
But then there’s the 2010 UCSF study of 91,000 men. It found surgery gave better survival-especially for high-risk patients. At 15 years, 62% of surgical patients were alive versus 52% of radiation patients. Why the difference? ProtecT mostly studied low-risk cases. UCSF included high-risk men, where cancer is more aggressive and harder to control with radiation alone.
So here’s what matters: your risk level. If you have low-risk prostate cancer, both options work well. If you’re high-risk, surgery might give you a better shot at long-term survival. But radiation still works-and it avoids the immediate physical trauma of surgery.

Lung Cancer: Surgery Still Leads-But Radiation Is a Lifeline
For non-small cell lung cancer (NSCLC), surgery remains the gold standard-if you’re healthy enough. The 2022 National Cancer Database study showed surgery patients lived longer: 71.4% survived five years versus 55.9% for SBRT.But here’s the critical detail: SBRT was used mostly for patients who couldn’t have surgery. Older patients. People with heart disease. Those with poor lung function. When you compare only patients who were medically eligible for both, the gap shrinks. And for someone who can’t have surgery, SBRT is life-changing. It’s not perfect-but it’s the best alternative.
That’s why guidelines say: if you’re operable, go for surgery. If you’re not, SBRT is your next best option. And for some, it’s the only option.
Side Effects: What You’re Really Trading
This isn’t just about survival. It’s about quality of life.Men who choose surgery often trade cancer control for urinary and sexual function. Radiation trades those for bowel issues. Neither is easy.
One man I spoke with-a 68-year-old retired teacher from Sydney-chose radiation for his prostate cancer because he didn’t want to risk incontinence. He said, "I’d rather have a little rectal discomfort than have to wear pads for the rest of my life." He’s been fine for five years. His bowel issues? Manageable with diet changes.
Another patient, 62, chose surgery because he hated the idea of daily radiation for months. He had robotic surgery, recovered in six weeks, and now plays golf. But he still uses a pad at night. "It’s a trade-off," he told me. "I chose the one I could live with."
There’s no right answer. Only the answer that fits your life.
What Experts Really Say
The National Comprehensive Cancer Network (NCCN) and the American Society of Clinical Oncology both say the same thing: talk to both a surgeon and a radiation oncologist before deciding.Why both? Because each specialist sees the problem through their own lens. A surgeon sees the tumor and thinks, "I can take this out." A radiation oncologist sees the same tumor and thinks, "I can destroy it without cutting." Neither is wrong. But neither has the full picture.
Dr. Christopher King from Cedars-Sinai says, "Radiation isn’t what people imagine." He’s right. Modern radiation is precise. It’s not blasting your whole body. It’s like a sniper, not a shotgun.
And Dr. Matthew Cooperberg from UCSF, who led that landmark 2010 study, says this: "There’s relatively little high-quality evidence to guide treatment." Translation? We’re still learning. Your choice should be based on your values-not just statistics.
Practical Realities: Time, Travel, and Your Life
Let’s talk logistics.Surgery? You’re out of commission for 2-6 weeks. But it’s over. One big event. Then you heal.
Radiation? You’re in treatment for 7-9 weeks. That’s 35-45 trips to the clinic. If you live in a rural area, or don’t have a car, that’s a huge burden. Some people quit because they can’t keep up.
SBRT for lung cancer? Five visits. No hospital stay. You can work, drive, take your dog for walks. It’s easier on your schedule. But it’s not for everyone.
And don’t forget: radiation can’t be repeated easily in the same area. If the cancer comes back, your options are limited. Surgery? You can sometimes have a second operation, depending on the situation.
What’s Next? New Options on the Horizon
Focal therapy for prostate cancer-targeting only part of the gland-is being tested in trials like PARTICLE (NCT03851707). Results are expected in 2025. If it works, it could mean fewer side effects than whole-gland treatment.Proton beam therapy is another emerging option. It delivers radiation with even less damage to surrounding tissue. But it’s expensive and not widely available.
For now, surgery and radiation remain the two pillars. The rest? Still experimental.
How to Decide
Here’s a simple way to think about it:- Know your cancer stage and risk level. Low-risk? Both options are strong. High-risk? Surgery often has the edge.
- Ask yourself: What side effects can you live with? Urinary leakage? Bowel issues? Erectile dysfunction? Which one scares you more?
- Can you handle 9 weeks of daily treatments? Or do you need it over fast?
- Are you healthy enough for surgery? Heart disease? Lung problems? Diabetes? Those might rule out surgery.
- Get both opinions. Don’t just talk to one doctor. See a surgeon AND a radiation oncologist. Ask them: "If this were your dad, what would you do?"
There’s no perfect choice. But there is a right one-for you.
Is radiation better than surgery for prostate cancer?
Neither is universally better. For low-risk prostate cancer, both offer nearly identical survival rates. Surgery has a slightly lower chance of cancer returning, but causes more urinary and sexual side effects. Radiation avoids surgery but can lead to bowel problems over time. The best choice depends on your risk level, age, and which side effects you’re willing to accept.
Can radiation be used instead of surgery for lung cancer?
Yes-for patients who can’t have surgery due to age, heart disease, or poor lung function. For those who are healthy enough, surgery still offers the best survival rates. But for inoperable patients, SBRT (stereotactic body radiation therapy) is a proven alternative with 40-50% five-year survival for early-stage lung cancer.
How long does radiation treatment take compared to surgery?
Surgery is usually a one-time event lasting a few hours, with recovery over 4-8 weeks. Traditional radiation for prostate cancer requires daily sessions for 7-9 weeks (about 35-45 visits). SBRT for lung or prostate cancer cuts that to just 1-5 sessions over 1-2 weeks, with little to no recovery time.
Do I need both surgery and radiation?
Sometimes. For high-risk prostate cancer, radiation is often combined with hormone therapy after surgery. For some lung cancers, radiation may be used after surgery if cancer cells are found near the edges of the removed tissue. But you don’t usually do both as primary treatments. The choice is typically one or the other.
What’s the most important factor in choosing between them?
Your personal values. Survival rates are similar in many cases. What matters more is which side effects you’re willing to live with-urinary leakage, bowel issues, sexual dysfunction, or the burden of daily treatments for weeks. Talk to both specialists. Ask yourself: "What kind of life do I want after treatment?"

Colin Pierce
January 27, 2026 AT 20:46Surgery gave me my life back after prostate cancer, but I won't pretend it was easy. Six weeks of no lifting, no driving, and nights spent in sweatpants. But I'm here, golfing again, and I didn't have to schedule my life around a clinic for two months. If you're healthy enough, go for the one-time fix. Radiation feels like a slow drip of stress.
Sue Latham
January 28, 2026 AT 18:28Ugh, I can't believe people still think surgery is the 'gold standard.' It's 2025. We've got SBRT, proton therapy, focal ablation-why are we still cutting people open like it's 1998? If your doctor pushes surgery without mentioning newer options, they're stuck in the past. #ModernMedicine
fiona vaz
January 29, 2026 AT 04:17My mom chose radiation for her early-stage lung cancer. She lived 30 minutes from the center, so she drove herself every day. It was exhausting, but she never had to be hospitalized. She said the fatigue was worse than the fear. Now she's five years clear, and her only issue is occasional dry cough. It’s not glamorous, but it worked.
Howard Esakov
January 30, 2026 AT 17:15Let’s be real-radiation is just a corporate cash grab. Hospitals make more money off 35 visits than one surgery. And don’t get me started on how they upsell you on 'premium' proton beams. Meanwhile, surgeons are the real heroes who actually remove the problem. Stop romanticizing radiation. It’s a Band-Aid with a price tag.
Kathy Scaman
February 1, 2026 AT 05:51I had both. Surgery first, then radiation because margins were close. It was brutal. But I’m alive. And honestly? I’d do it again. The key isn’t picking one over the other-it’s picking the team that listens to you. My oncologist cried when I told her I wanted to keep working. She made sure I could.
Lexi Karuzis
February 2, 2026 AT 18:57Wait-did you know the FDA approved SBRT using data from a 2018 study that was later retracted? And radiation oncologists are paid per session? There’s a conflict of interest here. Also, the 10-year bowel damage stats? They’re buried in footnotes. They don’t want you to know how many people end up on colostomy bags after 'precision' radiation. Wake up!
James Dwyer
February 2, 2026 AT 22:25My uncle picked radiation because he didn’t want to be laid up for months-he was still running his small business. Five sessions, back to work in three days. No incontinence, no ED. Just a little tired. He’s been fine for seven years. Sometimes the simplest choice is the right one.
Anna Lou Chen
February 3, 2026 AT 16:18The entire paradigm of localized cancer treatment is a reductive ontological fallacy. You’re not choosing between 'surgery' and 'radiation'-you’re negotiating a biopolitical surrender to a medical-industrial complex that pathologizes embodiment. Focal therapy, while statistically marginal, represents a post-humanist rupture in the Cartesian dichotomy of cutting versus zapping. The real question isn’t 'which modality?' but 'which epistemology of healing do you consent to?'
Rhiannon Bosse
February 4, 2026 AT 17:12Oh my god, I just read this whole thing and I’m crying. Like, seriously. I had radiation for breast cancer and now I have this weird scar that burns in the cold. And my husband won’t touch me. But at least I didn’t lose my boob. So I guess I won? 😭 No, wait-what even IS winning? This system is designed to make you feel like you chose, but really you just survived the gauntlet. I’m not okay.
Brittany Fiddes
February 5, 2026 AT 01:56Let’s be honest-Americans are too lazy for surgery. Radiation is the 'easy' option. In the UK, we still believe in getting it done properly. Cut it out, fix it, move on. No 9-week marathon of clinic visits. We don’t pamper cancer. We eradicate it. If you can’t handle a 3-hour operation, maybe you shouldn’t be fighting it at all.