Understanding Capecitabine and Its Role in Cancer Treatment
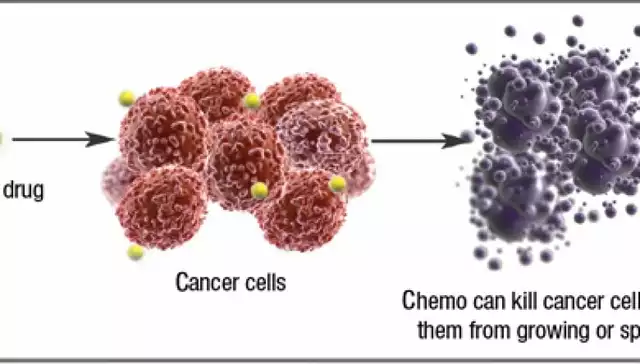
Capecitabine is an oral chemotherapy drug that has been successfully used in the treatment of various cancers, such as colorectal cancer and breast cancer. It is a prodrug, meaning that it is converted into its active form, 5-fluorouracil, within the body. This conversion occurs primarily in cancer cells, helping to minimize damage to healthy cells. In this section, we will delve deeper into the nature of capecitabine and how it works as a cancer treatment.
How Capecitabine Affects the Immune System
While the primary role of capecitabine is to target and kill cancer cells, its impact on the immune system is also significant. As the immune system is responsible for fighting off infections and diseases, understanding how capecitabine affects it is crucial in evaluating its overall effectiveness and safety. In this section, we will explore the various ways in which capecitabine interacts with the immune system.
Boosting the Immune Response to Cancer Cells
One of the ways capecitabine can impact the immune system is by enhancing its ability to recognize and attack cancer cells. Some studies have shown that capecitabine can increase the expression of certain proteins on the surface of cancer cells, making them more visible to the immune system. This can result in a more effective immune response against the cancer, potentially improving the overall outcome of the treatment.
Capecitabine's Effect on Immune Cell Populations
Another aspect of capecitabine's impact on the immune system is its influence on the populations of various immune cells. Some research has shown that capecitabine can affect the levels of specific immune cells, such as T-cells, B-cells, and natural killer cells. These changes in immune cell populations can have both positive and negative consequences, which will be discussed in further detail in this section.
Reducing Inflammation and Improving Immune Function
Chronic inflammation is a common issue in cancer patients and can contribute to a weakened immune system. Capecitabine has been shown to have anti-inflammatory properties, which can help reduce inflammation and improve immune function. By alleviating inflammation, capecitabine may help support the immune system's ability to fight off infections and other complications that can arise during cancer treatment.
Potential Side Effects on the Immune System
While capecitabine can have beneficial effects on the immune system, it can also cause some side effects. One potential side effect is the suppression of bone marrow function, which can lead to a decrease in the production of immune cells. This can result in a weakened immune system and an increased risk of infections. In this section, we will discuss the various side effects that can be experienced by patients undergoing treatment with capecitabine.
Managing Immune-Related Side Effects of Capecitabine
It is essential for patients and healthcare providers to be aware of the potential immune-related side effects of capecitabine and implement strategies to manage them effectively. This can include regular blood tests to monitor immune cell levels, adjusting the dosage of capecitabine, and providing supportive care to help manage symptoms. In this section, we will explore various strategies for managing the immune-related side effects of capecitabine treatment.
Combining Capecitabine with Immunotherapy
Immunotherapy is a rapidly evolving field of cancer treatment that aims to harness the power of the immune system to fight cancer. Some studies have suggested that combining capecitabine with immunotherapy drugs could enhance the immune system's response to cancer cells and improve treatment outcomes. In this section, we will discuss the potential benefits and challenges of combining capecitabine with immunotherapy treatments.
Capecitabine in the Context of Personalized Cancer Treatment
As the field of cancer treatment continues to advance, personalized medicine is becoming increasingly important. Understanding how capecitabine impacts the immune system can help tailor treatment plans to individual patients, potentially improving outcomes and minimizing side effects. In this section, we will discuss the importance of considering immune system factors when developing personalized cancer treatment plans involving capecitabine.
Conclusion: The Complex Relationship Between Capecitabine and the Immune System
In conclusion, capecitabine can have a significant impact on the immune system, with both positive and negative consequences. By understanding these effects, healthcare providers can develop more effective and personalized treatment plans for cancer patients. As research continues in this area, we can hope to gain a better understanding of capecitabine's role in cancer treatment and how it can be combined with other therapies to improve patient outcomes.


Mark Anderson
April 27, 2023 AT 18:05Wow, the way capecitabine can double‑tap the immune system is quite the kaleidoscope of effects. It's not just a silent assassin on tumor cells; it also paints the battlefield for T‑cells and NK cells. The anti‑inflammatory brushstroke it adds can soothe the chronic fire that cancers often stoke. Of course, like any powerful pigment, a splash too much can bleach the bone marrow, leading to a paler immune landscape. Overall, this chemo painter offers both vibrant hues and stark shadows, making personalized palettes essential.
Shouvik Mukherjee
April 28, 2023 AT 10:20It's wonderful to see how capecitabine can be a bridge between chemotherapy and immunology. By gently nudging immune cells into action, it helps patients feel more supported in their treatment journey. Encouraging clinicians to monitor blood counts regularly can ensure we catch any dips early. Together, we can foster a collaborative environment where the drug's benefits shine while its risks are managed thoughtfully.
Ben Hooper
April 29, 2023 AT 02:26Capecitabine converts to 5‑FU inside tumor cells. This limits damage to healthy tissue. Immune cell counts can shift during therapy. Monitoring is key.
Marjory Beatriz Barbosa Honório
April 29, 2023 AT 19:06Thinking about those shifts, it's like a dance where the drug leads but the immune system follows. The increased expression of tumor antigens can really spark a lively waltz with T‑cells, making the fight more coordinated. Yet, we must stay mindful of the rhythm, as over‑synchronizing might tire the marrow. A balanced choreography keeps both dancers healthy and effective. Keep the beat steady, and the audience – our patients – will applaud.
G.Pritiranjan Das
April 30, 2023 AT 11:13Capecitabine helps the immune system but watch blood counts.
Karen Wolsey
May 1, 2023 AT 05:00Oh great, another chemo that pretends to be a superhero for the immune system. Sure, it might boost some markers, but then it quietly whacks the bone marrow when you’re not looking. Nothing says "I care" like a side‑effect that forces you into isolation.
Trinity 13
May 1, 2023 AT 21:40Let's dive deep into the philosophical currents that capecitabine stirs within the immune tapestry. First, consider the notion that a drug can act as both a catalyst and a gatekeeper – it unlocks hidden antigens while simultaneously narrowing the battlefield by suppressing certain leukocytes. This duality echoes the ancient paradox of fire: it provides warmth and illumination, yet it can also consume everything in its path. When capecitabine transforms into 5‑FU, it performs a molecular alchemy that is almost poetic, converting an inert prodrug into an aggressive agent that selectively targets rapidly dividing cells, sparing most quiescent tissues – at least in theory. The reality, however, is that the immune system is not a static entity; it's a dynamic orchestra of cells, cytokines, and signals, each reacting to the drug's presence in a cascade of feedback loops. For instance, the upregulation of MHC class I on tumor cells can enhance recognition by cytotoxic T‑lymphocytes, essentially painting a target on the cancer's surface. Yet the same drug may also diminish the proliferative capacity of naïve T‑cells in the bone marrow, a grim reminder that the very engine of renewal can be throttled by the therapeutic assault.
Moreover, the anti‑inflammatory properties of capecitabine can be seen as a double‑edged sword. On one side, reducing chronic inflammation may alleviate the immunosuppressive milieu that tumors exploit, thereby restoring a more vigilant immune surveillance. On the other side, inflammation is a vital signal for immune activation; dampening it too much could blunt the recruitment of effector cells to the tumor microenvironment. This tension mirrors the existential balance between order and chaos, a theme explored by philosophers from Heraclitus to modern thinkers. In practical terms, clinicians must walk a tightrope, calibrating dosage schedules to maximize tumoricidal effects while preserving enough immune vigor to fend off opportunistic infections. Regular peripheral blood monitoring, dose adjustments, and supportive care like growth factor administration become the pragmatic rituals that translate theory into survivable reality.
When we consider combination therapies, the narrative becomes even richer. Pairing capecitabine with checkpoint inhibitors, for example, leverages its antigen‑revealing capabilities while unleashing the brakes on T‑cell activity. This synergistic strategy aims to convert a 'cold' tumor environment into a 'hot' one, primed for immune attack. Yet this alliance is not without challenges – the risk of heightened autoimmunity rises, and the long‑term consequences on immune homeostasis remain partially unknown. As we march toward personalized oncology, the interplay between drug pharmacodynamics, patient genetics, and immune profiling will dictate who benefits most from such regimens. In essence, capecitabine serves as a microcosm of modern cancer therapy: a potent, multifaceted tool that demands nuanced understanding, careful stewardship, and an appreciation of the delicate balance it imposes on the human immune system.
Rhiane Heslop
May 2, 2023 AT 15:43Our nation deserves treatments that fortify, not those that silently erode the marrow. Capecitabine’s immune tweaks must be scrutinized with patriotic rigor.
Dorothy Ng
May 3, 2023 AT 09:46Capecitabine’s impact on T‑cells is noteworthy; maintaining balance is vital.
Justin Elms
May 4, 2023 AT 03:50It’s cool that capecitabine can help the immune system while fighting cancer it makes treatment easier for patients
Jesse Stubbs
May 4, 2023 AT 21:53What a tragic waste of potential.
Melissa H.
May 5, 2023 AT 15:56Interesting how capecitabine can boost antigen visibility 😊 but you gotta watch those blood counts though!
Edmond Abdou
May 6, 2023 AT 10:00Great point! Keeping an eye on immune markers while on capecitabine can make a big difference 😊
Sydnie Baker
May 7, 2023 AT 04:03From a pharmacodynamic perspective, capecitabine exemplifies a prodrug paradigm with nuanced immunomodulatory sequelae. Its enzymatic conversion to 5‑FU within neoplastic microenvironments precipitates upregulation of MHC‑I complexes, thereby augmenting neoantigen presentation. Concurrently, the myelosuppressive profile necessitates vigilant hematologic surveillance to preempt neutropenic complications. In sum, this agent straddles the axis of efficacy and immunological perturbation.
Benjie Gillam
May 7, 2023 AT 22:06Capecitabine's chemo‑logic is like a double‑edged sword, wielded with precision, yet demanding rigorous monitoring of lymphocyte dynamics to balance oncologic eradication with immunological integrity.
Naresh Sehgal
May 8, 2023 AT 16:10Listen up! Capecitabine can fire up your immune response but don’t be lazy-track those labs, adjust doses, and stay on top of side‑effects. This isn’t a game; it’s a battle, and you need to be aggressive in managing it. Push forward, keep the momentum, and you’ll see better outcomes!
Poppy Johnston
May 9, 2023 AT 10:13Just a heads‑up, if you’re on capecitabine, stay chill and keep an eye on your blood work. It helps keep the immune system in check without stressing yourself out.
Johnny VonGriz
May 10, 2023 AT 04:16Hey folks, great discussion here. I’d add that patient education on potential immune side‑effects is key. When you know what to look for-like unexpected fevers or fatigue-you can act fast. Also, coordinating with your oncologist about timing of immunotherapy combos can make a big difference. Let’s keep the conversation rolling and share any personal experiences you’ve had.
Real Strategy PR
May 10, 2023 AT 22:20Honestly, the so‑called “immune boost” from capecitabine is overhyped. It’s just a marketing gimmick.