Pancreatic Blockage Emergency Checker
Check Your Symptoms
This tool helps you determine if your symptoms require immediate medical attention. Based on the latest medical guidelines for pancreatic duct blockage.
Select symptoms to check if you need urgent care.
Quick Takeaways
- Regular monitoring catches complications early, when treatment works best.
- Blood work, imaging, and symptom reviews form the backbone of each visit.
- Follow‑up frequency depends on blockage severity, underlying disease and treatment plan.
- Know the warning signs - sudden pain, jaundice, fever - that demand urgent care.
- Simple lifestyle tweaks (low‑fat diet, staying hydrated) help keep the pancreas stable between appointments.
What Is Pancreatic Duct Blockage?
Pancreatic duct blockage is a condition where the main channel that carries digestive enzymes from the pancreas to the duodenum becomes narrowed or completely obstructed. The blockage may stem from scar tissue, gallstones, tumors or chronic inflammation. When the duct can’t drain properly, enzymes back up, leading to inflammation (pancreatitis), pain, and over time, loss of pancreatic function.
The pancreas itself is a gland located behind the stomach that produces both digestive enzymes and hormones like insulin. Pancreas is a mixed exocrine‑endocrine organ responsible for digestion and blood‑sugar regulation. A blocked duct turns this finely tuned system into a ticking time‑bomb, which is why doctors stress consistent follow‑up.
Pancreatic duct blockage can silently worsen; you might feel fine one week and experience severe pain the next. That unpredictability makes scheduled checkups a lifeline.
Why Regular Checkups Matter
Imagine you own a car with a clogged fuel line. You could keep driving, but each mile raises the risk of engine failure. The same logic applies to the pancreas. Regular appointments let your care team spot early signs of worsening obstruction, infection or the scary transition to cancer.
Key benefits of routine monitoring include:
- Detecting new stones or tissue overgrowth before they cause severe blockage.
- Assessing whether an existing stent (if you have one) remains patent.
- Tracking blood markers like amylase, lipase and liver enzymes that flag inflammation.
- Adjusting medication dosages, such as pancreatic enzyme replacements, based on current digestion efficiency.
- Providing timely referrals to a specialist if the disease progresses.
Studies from major gastroenterology centers in 2023 show that patients who stick to a 3‑month imaging schedule experience a 40% reduction in emergency hospital admissions compared with those who see a doctor only when symptoms flare.
Typical Follow‑up Schedule
There isn’t a one‑size‑fits‑all calendar, but most clinicians follow a tiered timeline:
- First month after diagnosis or intervention: A baseline visit to review symptoms, run a full blood panel, and perform an initial imaging study.
- Every 3months for the first year: Repeat blood work and a non‑invasive imaging test (usually MRI or MRCP) to see if the blockage is stable.
- Every 6months in years2‑3: If the duct remains clear, the interval can stretch, but a repeat visit is still essential.
- Annual review thereafter: Long‑term patients often shift to an annual scan, unless new symptoms appear.
The exact rhythm depends on factors like:
- Underlying cause - gallstones may need tighter surveillance than a benign stricture.
- Presence of a stent - metal or plastic tubes can clog, demanding more frequent checks.
- Co‑existing conditions - diabetes, chronic pancreatitis or a history of pancreatic cancer changes the risk profile.
All appointments are usually coordinated by a gastroenterologist a physician who specializes in digestive system disorders, including pancreatic disease. In complex cases, a hepatobiliary surgeon may join the team.
What Happens During a Checkup?
Each visit follows a predictable pattern, helping you know what to expect and how to prepare.
- Symptom review: You’ll discuss pain intensity, any new jaundice, changes in stool colour, or unexplained weight loss.
- Physical exam: The doctor palpates the abdomen, checks for tenderness and may listen for abnormal bowel sounds.
- Blood tests: A panel typically includes amylase, lipase, bilirubin, alkaline phosphatase, and glucose levels. Elevated enzymes hint at ongoing inflammation.
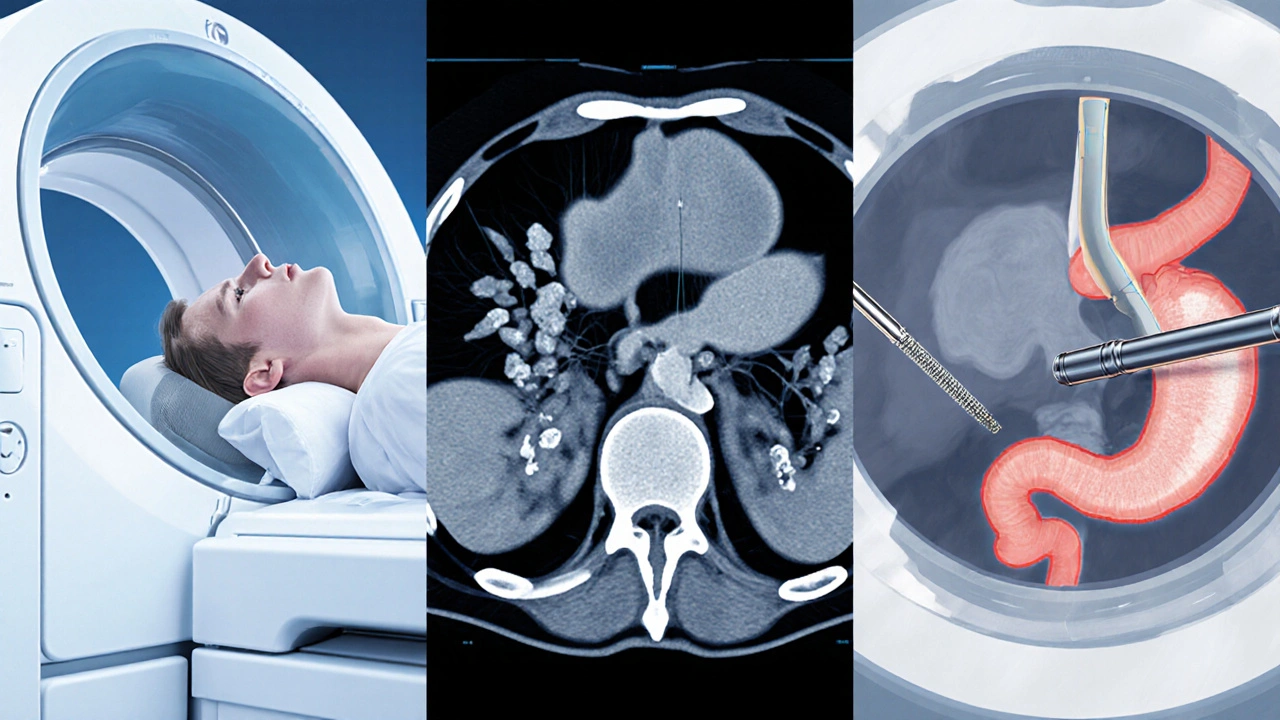
- Imaging study: Depending on the stage, you may get an MRI, CT scan, or an endoscopic ultrasound (EUS). The choice balances detail, radiation exposure and cost.
- Discussion of treatment plan: If imaging shows progression, options like repeat ERCP, stent replacement, or surgical bypass are explored.
All results are usually reviewed with you on the same day or within a few days, so you can make informed decisions quickly.
Imaging Options: MRI vs. CT vs. ERCP
Choosing the right imaging tool is a balance of accuracy, invasiveness and availability. Below is a quick side‑by‑side look.
| Modality | Detail Level | Invasiveness | Radiation | Typical Use |
|---|---|---|---|---|
| MRI (Magnetic Resonance Imaging) | High - excellent soft‑tissue contrast | Non‑invasive | None | Routine monitoring, detecting subtle ductal changes |
| CT Scan (Computed Tomography) | Moderate - good for calcifications, quick | Non‑invasive | Yes (ionizing) | Acute pain episodes, evaluating complications |
| ERCP (Endoscopic Retrograde Cholangiopancreatography) | Very high - visualizes duct directly and allows intervention | Invasive (endoscopic) | Minimal (contrast use) | Therapeutic stent placement, stone removal, biopsy |
Most patients start with MRI for routine follow‑up because it’s radiation‑free. If a blockage worsens or symptoms spike, a CT can quickly rule out perforation or abscess. ERCP is reserved for therapeutic actions - it’s the only tool that can physically clear or bypass the obstruction.
Managing Symptoms Between Visits
Even with perfect appointments, day‑to‑day life can feel challenging. Here are practical tips that many patients find helpful:
- Low‑fat diet: Fat stimulates enzyme production, which can aggravate a blocked duct. Aim for <10g of fat per meal and choose lean proteins, whole grains and plenty of vegetables.
- Stay hydrated: Water helps keep secretions thin, reducing the chance of sludge forming.
- Enzyme supplements: If your doctor prescribed pancreatic enzymes, take them with every meal and snack to aid digestion.
- Gentle activity: Light walking improves circulation without stressing the abdomen.
- Pain diary: Record pain intensity, timing and triggers. This log is gold for your next appointment.
These habits don’t replace medical care, but they shore up the gaps between checkups and can delay complications.
Red Flags: When to Seek Immediate Care
Even with a solid follow‑up plan, some situations demand urgent attention. Call your gastroenterologist or head to the emergency department if you notice:
- Sudden, severe abdominal pain that doesn’t ease with usual pain meds.
- Yellowing of the skin or eyes (jaundice), indicating bile flow blockage.
- Fever above 38°C (100.4°F) combined with abdominal tenderness - a possible infection.
- Rapid weight loss (>5% in a month) or severe weakness.
- Vomiting that contains bile or blood.
Prompt treatment can prevent sepsis, organ failure, or the need for more extensive surgery.
Frequently Asked Questions
How often should I get imaging if my duct is mildly blocked?
For mild, stable blockages most specialists recommend an MRI every three months during the first year, then every six months if nothing changes. Your doctor may stretch the interval based on blood test trends.
Can lifestyle changes reverse a blockage?
Lifestyle tweaks can reduce inflammation and prevent new stones from forming, but they rarely dissolve an existing obstruction. They are still vital for overall pancreatic health and to keep symptoms manageable.
What is the difference between ERCP and MRCP?
ERCP is an endoscopic, minimally invasive procedure that lets doctors inject contrast, view the duct directly, and perform interventions (like stent placement). MRCP (Magnetic Resonance Cholangiopancreatography) is a non‑invasive MRI technique that creates detailed images of the ducts but cannot treat them.
Will I need surgery eventually?
Surgery is reserved for cases where the blockage can’t be cleared endoscopically, or when there’s a suspicious mass. Many patients avoid surgery by staying on a strict follow‑up and getting timely ERCPs.
How do I prepare for an MRI of the pancreas?
Usually you’ll be asked to fast for 4-6 hours before the scan to reduce bowel motion. If you have a metal implant, inform the technologist - some devices are MRI‑compatible, others aren’t.


Craig Stephenson
October 14, 2025 AT 14:42Regular check‑ups really keep the pancreas on track.
Eve Perron
October 14, 2025 AT 21:39When we talk about pancreatic duct blockage, the underlying pathophysiology is as intricate as any organ system in the human body, demanding our full attention.
The pancreas, a dual‑purpose gland, not only secretes digestive enzymes but also regulates glucose homeostasis through insulin, so any obstruction can have cascading metabolic effects.
Because the duct serves as the conduit for those enzymes, a blockage creates a bottleneck that forces the enzymes to back‑up, leading to autodigestion and inflammation, which we clinically recognize as pancreatitis.
Studies published in 2023 demonstrate that a systematic imaging schedule, particularly using MRI or MRCP at three‑month intervals, reduces emergent admissions by nearly forty percent.
This statistic underscores the value of proactive surveillance; catching a nascent stone or stricture before it becomes symptomatic can spare patients from pain, hospitalization, and costly interventions.
Moreover, routine blood panels-amylase, lipase, bilirubin, alkaline phosphatase-serve as biochemical sentinels, often flagging subtle changes that imaging alone might miss.
When these labs trend upward, clinicians can adjust enzyme replacement dosages or schedule an earlier endoscopic assessment, thereby averting a crisis.
From a practical standpoint, patients should view each appointment as a checkpoint, much like a pit stop in a race; neglecting it can result in a catastrophic engine failure.
The recommended follow‑up cadence varies: initially monthly, then every three months for the first year, followed by six‑monthly intervals, and eventually annual reviews, contingent upon disease stability.
Patients with a stent in place may require tighter monitoring because stent occlusion is a common cause of recurrent blockage.
Lifestyle modifications, such as adhering to a low‑fat diet and maintaining adequate hydration, can complement medical management, reducing the formation of new stones.
Nevertheless, these measures rarely dissolve an existing obstruction; they primarily mitigate inflammation and prevent secondary complications.
In the event of acute symptoms-sudden severe abdominal pain, jaundice, fever exceeding 101°F, or vomiting of bile-immediate medical attention is paramount, as delays can precipitate sepsis or organ failure.
Emergency departments can perform rapid CT scanning to evaluate for perforation or abscess, while gastroenterology can arrange urgent ERCP for therapeutic intervention.
Thus, the synergy between scheduled maintenance and rapid response to red‑flag symptoms constitutes the cornerstone of optimal care for pancreatic duct blockage patients.
Finally, patients should maintain an open line of communication with their care team, reporting any new or worsening symptoms without hesitation.
Josephine Bonaparte
October 15, 2025 AT 04:36Look, you gotta keep up with those visits, otherwise you’re just playing roulette with your health – it’s definitely not worth the risk. I’ve seen too many people skip a scan and end up in the ER later, and that’s just avoidable.
Brian Lancaster-Mayzure
October 15, 2025 AT 11:32From a practical side, the imaging schedule can be adjusted if your labs stay stable. Just keep the lines of communication open with your gastro team.
mitch giezeman
October 15, 2025 AT 18:29The routine blood work is a cheap early warning system; don’t ignore subtle rises in lipase or bilirubin.
Kelly Gibbs
October 16, 2025 AT 01:26Stent patency checks are essential.
Stephanie Pineda
October 16, 2025 AT 08:22Life’s like a river of enzymes, sometimes calm, sometimes tumultuous; keeping the flow smooth is an art and a science.
Anne Snyder
October 16, 2025 AT 15:19Utilizing MRCP for non‑invasive surveillance leverages high‑resolution cholangiography without radiation exposure, which is optimal for longitudinal monitoring.
Rebecca M
October 16, 2025 AT 22:16Precise lab trends; early detection of enzymatic spikes prevents downstream complications.
Bianca Fernández Rodríguez
October 17, 2025 AT 05:12Theres no need for that many appointments, they just waste time and money. Plus, the scans can be i nc o m p l e t e.
Patrick Culliton
October 17, 2025 AT 12:09I dont buy the hype about constant monitoring; if you feel fine, why bother?
Andrea Smith
October 17, 2025 AT 19:06I sincerely commend the thoroughness of this guide; it offers a clear, evidence‑based pathway for patients navigating pancreatic duct obstruction.
Gary O'Connor
October 18, 2025 AT 02:02Sounds solid, especially the MRI‑first approach.
Justin Stanus
October 18, 2025 AT 08:59It’s hard to stay positive when the pancreas keeps acting up.