Penile surgery is a subspecialty of urologic surgery that handles structural and functional issues of the penis, including the management of complications from penile prosthesis implantation. It combines precise dissection, tissue preservation, and device‑specific techniques to restore comfort and sexual function.
Why penile prosthesis complications matter
Implantable devices have transformed treatment for severe erectile dysfunction (ED), but about 10‑15% of men experience problems within the first three years. The most frequent issues are infection, mechanical failure, and erosion into adjacent tissues. Left untreated, these complications can lead to chronic pain, loss of penile length, and psychological distress.
Key players in the complication landscape
Penile prosthesis is a medical device-either inflatable (three‑piece) or malleable (semi‑rigid)-designed to mimic a natural erection when activated. It is the third‑line therapy after oral PDE5 inhibitors and vacuum devices.
Erectile dysfunction is the inability to achieve or maintain an erection sufficient for sexual activity. In severe, refractory cases, penile prosthesis implantation offers a permanent solution.
Infection refers to bacterial colonisation of the implant pocket, often presenting with redness, swelling, and fever. Reported rates range from 1‑3% in virgin implants to over 10% after revision procedures.
Mechanical failure encompasses pump malfunction, reservoir leakage, or rod fracture, leading to loss of rigidity or uncontrolled inflation.
Urologist is the specialist who performs implantation, monitors outcomes, and decides on corrective surgery when complications arise.
When surgery becomes necessary
Not every complication needs an operation. Mild, early‑stage infection may resolve with targeted antibiotics and device‑preserving drainage. However, the following scenarios usually trigger surgical intervention:
- Confirmed infection with purulence or systemic signs.
- Device erosion into the urethra or corpora cavernosa.
- Persistent mechanical failure despite conservative troubleshooting.
- Patient‑reported loss of device function that impairs sexual activity.
In each case, the urologist evaluates tissue health, infection severity, and the patient’s expectations before recommending a specific surgical pathway.
Surgical options: explantation, revision, and salvage
Three main approaches address prosthesis complications. Choosing among them depends on infection status, device condition, and the amount of healthy tissue remaining.
| Procedure | Indication | Invasiveness | Success rate (rough estimate) | Typical recovery |
|---|---|---|---|---|
| Explantation | Severe infection, extensive tissue loss | High (device removal, extensive debridement) | 95% infection eradication | 4‑6 weeks before any re‑implant |
| Revision surgery | Mechanical failure, partial erosion, non‑infected malfunction | Medium (device replacement, limited dissection) | 80‑90% functional restoration | 2‑3 weeks |
| Salvage surgery | Early‑stage infection with viable tissue | Low‑to‑medium (device exchange + antibiotic irrigation) | 70‑85% device preservation | 1‑2 weeks |
These numbers come from multicenter registries published in 2023‑2024, which pooled outcomes of over 2,500 cases worldwide.
Salvage surgery: the tissue‑saving play
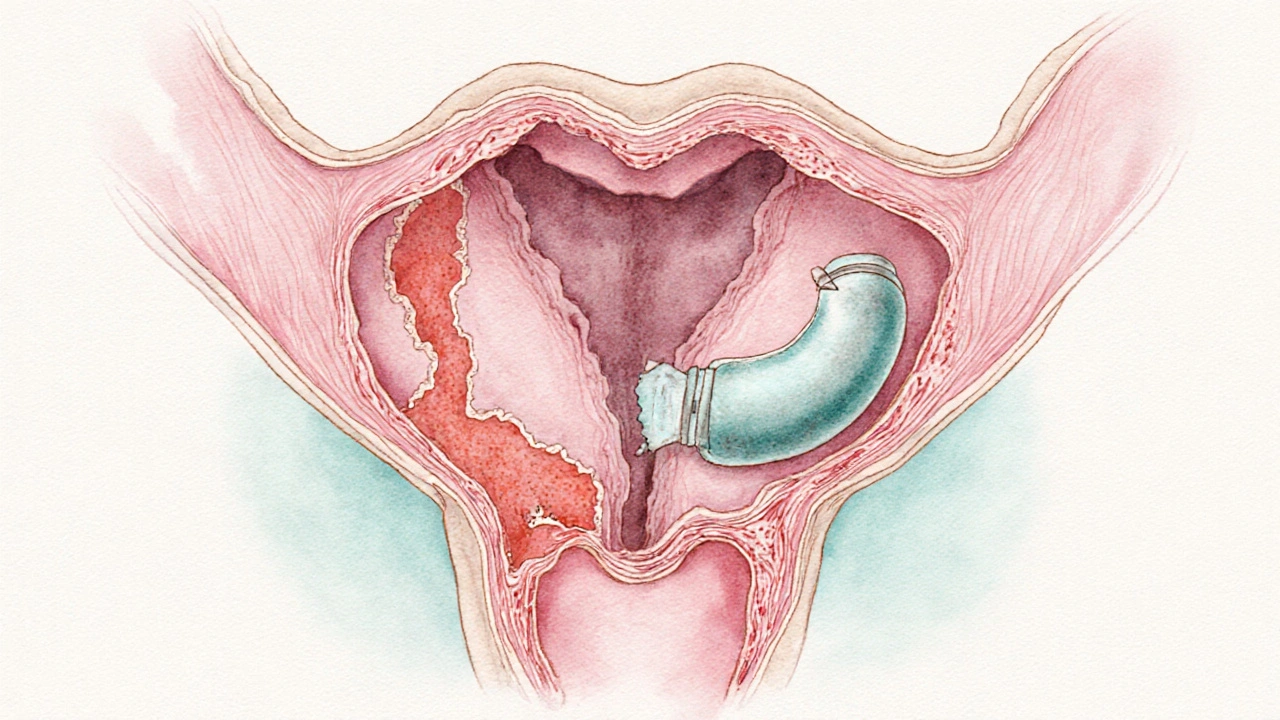
Salvage surgery is a device‑preserving technique performed when infection is caught early and the surrounding corpora cavernosa remain healthy. The surgeon removes the infected components, irrigates the pocket with antibiotic solution, and immediately implants a fresh device.
Key steps include:
- Incision through the previous scar (usually scrotal or penoscrotal).
- Careful extraction of the infected pump or cylinders.
- Extensive lavage with vancomycin‑gentamicin solution.
- Placement of a new prosthesis, often of the same type.
- Closed‑system drainage for 48‑72hours.
Success hinges on rapid antibiotic administration (within 6hours of diagnosis) and meticulous aseptic technique. Patients who avoid full explantation preserve penile length and avoid a second healing phase.
Revision surgery: fixing the broken parts
Revision surgery addresses mechanical faults, such as pump failure or cylinder fracture, without infection. The operation typically involves removing the defective component and inserting a new one while preserving the existing tubing and reservoir.
Advantages include a shorter operative time (often under 90minutes) and a lower risk of new infection because the original pocket remains intact. However, surgeons must assess whether scar tissue has compromised the corpora; excessive fibrosis may necessitate a full explantation instead.
Explantation: when removal is the only safe choice
Explantation is the complete removal of the prosthetic system, usually followed by a period of observation before any re‑implant. Indications include uncontrolled infection, extensive erosion into the urethra, or necrotic tissue that cannot support a new device.
After explantation, patients receive a course of broad‑spectrum antibiotics (often a combination of a third‑generation cephalosporin and metronidazole) for 2‑3weeks. Once the wound is clean and the corpora have re‑epithelialised, a delayed re‑implant can be planned, typically after 8‑12weeks.
Choosing the right path: decision criteria for the urologist
Every case is a balance of infection severity, tissue viability, patient motivation, and long‑term functional goals. A practical decision tree looks like this:
- If systemic infection or gross purulence → explantation.
- If localized infection <48hours old, good tissue health → salvage surgery.
- If no infection but device malfunction or limited erosion → revision surgery.
Shared decision‑making is essential. Studies from the International Society of Sexual Medicine show that patients who understand the trade‑offs (e.g., possible loss of length with explantation vs. higher preservation rates with salvage) report higher satisfaction, even if complications occur.
Post‑operative care and outcomes
Regardless of the chosen surgery, the recovery protocol shares core elements:
- Ice packs for the first 48hours to minimise swelling.
- Antibiotic prophylaxis tailored to culture results (usually a quinolone plus doxycycline).
- Delayed activation of the device-usually after 2weeks for revision, 4‑6weeks for salvage, and once the wound is fully healed after explantation.
- Routine follow‑up at 1, 3, and 6months, focusing on penile girth, rigidity scores (IIEF‑5), and psychological wellbeing.
Long‑term data indicate that 85% of patients who undergo successful revision or salvage report a return to satisfactory sexual activity within six months. Explantation followed by delayed re‑implant yields comparable satisfaction, but the overall timeline stretches to a year.
Emerging techniques and future directions
Research in 2024 introduced antimicrobial‑coated cylinders that reduce infection rates by up to 40%. Additionally, robotic‑assisted penile surgery is gaining traction in high‑volume centers, offering more precise dissection and potentially lower fibrosis rates.
Another promising avenue is the use of autologous platelet‑rich plasma (PRP) at the time of salvage to promote tissue healing and reduce scar formation. Early case series report faster recovery, though larger trials are needed.
Related concepts you may want to explore
Understanding penile prosthesis complications fits into a bigger picture of male sexual health. Readers often look next at:
- Erectile dysfunction therapies - oral medications, vacuum devices, and intracavernosal injections.
- Penile rehabilitation - post‑operative exercises and pelvic floor training that improve outcomes.
- Psychosexual counseling - addressing the emotional impact of device failure.
- Device technology trends - newer inflatable models with pressure‑sensing technology.
Each of these topics deepens the conversation about restoring confidence and intimacy after a prosthetic setback.
Frequently Asked Questions
Can a penile prosthesis infection be treated without removing the device?
In early, localized infections, a salvage surgery that exchanges the infected component while preserving the rest of the system can be successful. Success rates hover around 70‑85% if antibiotics start within six hours and tissue remains healthy.
What is the difference between revision surgery and explantation?
Revision surgery replaces the faulty part of the implant while keeping the rest of the device in place; it’s used for mechanical failures or minor erosion without infection. Explantation removes the entire system, usually because of severe infection or extensive tissue damage, and requires a healing period before any re‑implant.
How long does it take to return to sexual activity after a salvage procedure?
Patients typically wait 4‑6weeks for the wound to mature before activating the new device. Full confidence in performance often returns by the three‑month mark.
Are there any preventive measures to avoid prosthesis complications?
Prophylactic antibiotics at the time of implantation, strict sterile technique, and patient education about proper device handling dramatically lower infection risk. Selecting an antimicrobial‑coated prosthesis further reduces the odds.
What are the chances of losing penile length after explantation?
Length loss can occur if scar tissue contracts during the healing phase. Using tissue‑expanding grafts at the time of re‑implant or employing early physiotherapy helps preserve length for most patients.


Alex Iosa
September 27, 2025 AT 20:59It is deeply troubling how the medical device industry repeatedly downplays the true scale of infection risk associated with penile prostheses. The narrative presented to patients is often sanitized, obscuring the fact that a hidden cohort of men suffers chronic complications. One must question whether corporate lobbying influences the published success rates, a classic example of information control. Ethical practice demands transparent data so that individuals can make fully informed decisions about such invasive procedures.
Mark Conner
September 27, 2025 AT 21:15Yo, real talk – American guys need a solid fix, not some flimsy gadget that rips apart.
Abraham Gayah
September 27, 2025 AT 21:32Another snooze‑fest article about screws and silicone – yawn.
rajendra kanoujiya
September 27, 2025 AT 21:49While many hail these surgeries as routine, the reality is that the literature often omits the long‑term psychosocial fallout that patients endure. Studies from independent clinics have shown a markedly higher rate of dissatisfaction when the device is removed after infection. Moreover, the alleged 95% infection eradication after explantation ignores the subtle, lingering tissue inflammation that can compromise future implants. It's worth noting that some surgeons prefer a staged approach precisely to avoid the hidden pitfalls that mainstream papers gloss over. In short, the consensus you see is far from the whole picture.
Caley Ross
September 27, 2025 AT 22:05I’ve seen a few guys go through revision surgery and they’re back to normal fairly quickly. The recovery timeline they mention checks out with what I’ve observed in community forums.
Bobby Hartono
September 27, 2025 AT 22:22The thing about penile prosthesis complications is that they’re not just a medical footnote, they impact a man's sense of identity and intimacy in profound ways. When an infection sets in, the body launches an inflammatory cascade that can erode not only tissue but also confidence. Early recognition is key, because once purulence spreads, the options narrow dramatically. Surgeons who opt for salvage surgery must work in a sterile field, irrigating the pocket with antibiotic solution while preserving as much of the corpora as possible. This approach, when done within the critical six‑hour window, can save the device and maintain penile length, which many patients fear losing. However, the success of salvage hinges on the patient's overall health, especially diabetes control, which is often overlooked in hurried consultations. Antibiotic regimens vary, but a combination of vancomycin and gentamicin has become the de‑facto standard in many centers. Post‑operative drainage for 48‑72 hours helps prevent fluid accumulation that could seed new infection. The rehabilitation phase includes gentle stretching exercises to avoid scar contracture, something most post‑op instructions forget to highlight. In my experience, patients who receive thorough counseling about these steps report higher satisfaction scores. On the flip side, explantation, though drastic, is sometimes the only safe route when necrotic tissue is present, and the subsequent healing period can be lengthy. The emotional toll during this downtime should not be dismissed; many men experience depression, and partner support becomes crucial. Revision surgery, while less invasive than full explant, still carries a risk of new infection if scar tissue is not adequately addressed. This is why some urologists advocate for a staged revision, allowing the tissue to settle before implanting a fresh device. Overall, the decision matrix is complex, balancing infection severity, tissue viability, and the patient's desire to avoid another surgery. Ultimately, open communication between the surgeon and patient, coupled with diligent post‑operative care, forms the backbone of successful outcomes.
George Frengos
September 27, 2025 AT 22:39Thank you for laying out such a comprehensive overview; the emphasis on timely intervention and patient counseling is particularly valuable. Your points about the psychological impact align with what many of us have observed in practice. It’s also crucial to highlight the role of meticulous aseptic technique during salvage, as you described. I would add that multidisciplinary follow‑up, including mental health support, can further enhance recovery.
Charles Markley
September 27, 2025 AT 22:55From a biomechanical perspective, the failure modes of inflatable prostheses can be stratified into hydraulic leakage, actuator fatigue, and reservoir compromise. Recent finite‑element analyses suggest that cyclic loading beyond 10⁶ cycles precipitates micro‑fractures in the silicone elastomer matrix. Moreover, biofilm formation on the pump’s internal surfaces escalates resistance to standard antimicrobial regimens, necessitating adjunctive anti‑biofilm agents. In the context of salvage surgery, the osmolality of the irrigation solution exerts a modulatory effect on bacterial adherence, a nuance often omitted from clinical guidelines. Therefore, optimizing both mechanical integrity and microbiological milieu is paramount for durable outcomes. Integration of sensor‑enabled prosthetic platforms could herald a paradigm shift in early complication detection.
L Taylor
September 27, 2025 AT 23:12Interesting take on the biomechanics but the real issue is patient experience we need to ask why so many men feel abandoned after a failure the industry pushes new models faster than we can study long term outcomes and surgeons are left scrambling to keep up with tech upgrades while patients suffer the consequences
diego suarez
September 27, 2025 AT 23:29Complications are not rare and they can be serious. Choosing the right surgical path depends on infection severity and tissue health. A clear discussion with the doctor helps set realistic expectations.
Eve Perron
September 27, 2025 AT 23:45Indeed, the decision matrix you outlined is both nuanced and critical; each factor-be it systemic infection, localized purulence, or the extent of corporal fibrosis-demands careful quantification, and the surgeon must weigh them against patient aspirations, lifestyle considerations, and long‑term functional goals. Moreover, recent meta‑analyses have highlighted that early salvage, performed within the six‑hour window, correlates with higher device retention rates, a statistic that cannot be overstated. Nevertheless, one must not overlook the psychological sequelae, which, according to longitudinal surveys, affect up to thirty percent of patients post‑explantation; this underscores the necessity of integrating mental health support into postoperative protocols. The antibiotic regimen, typically vancomycin plus gentamicin, should be tailored to culture sensitivities, and the duration of drainage catheters must be calibrated to minimize seroma formation while preventing secondary infection. Finally, the role of patient education cannot be overstated-transparent discussions regarding potential complications, recovery timelines, and realistic outcomes foster trust and improve adherence to postoperative care plans.
Manno Colburn
September 28, 2025 AT 00:02The whole idea of a prosthetic implant is kind of mind blowing if you think about it, you got a foreign mechancial object living inside a delicate tissue. Yet most papers talk about success rates like it's all sunshine and rainbows, ignoring the gritty side effects like thier impact on self‑esteem. I read a case where a man had to go through three revisions because the pump kept jammin, and each surgery left more scar tissue. This scar buildup can actually make a future explantation even more dangerous, because the tissue becomes less pliable. Also, antibiotics are not a silver bullet; resistant bacteria can form biofilims that regular regimens cannot clear. Some surgeons suggest using an antibiotic‑impregnated envelope around the device, which seems promising but not yet widely adopted. Overall, the decision should involve not just the urologist but also the patient’s partner, because the emotional toll is huge. In short, dont just trust the headline numbers, dig deeper.
Namrata Thakur
September 28, 2025 AT 00:19I completely agree with your assessment; the overlooked aspects you mention often become the decisive factors in outcomes. Emphasizing partner involvement and clear communication can mitigate the emotional burden you described. Also, the use of antibiotic‑impregnated envelopes is gaining traction and may address the biofilm concerns you raised. Thank you for shedding light on these critical nuances.
Chloe Ingham
September 28, 2025 AT 00:35What most people fail to see is that the push for newer devices is driven by hidden corporate agendas, not patient welfare. The relentless marketing campaigns mask the very real risks you outlined, steering men toward a cycle of implantation and revision. Some say it’s about profit, and the data on unexplained complications certainly adds weight to that theory. It’s as if we’re being fed a polished narrative while the mess underneath is swept under the rug. Wake up, folks, the truth is buried in the fine print.
Mildred Farfán
September 28, 2025 AT 00:52Oh sure, because it’s always “just a little tweak” and suddenly everything’s back to normal. Right, like fixing a leaky faucet solves the whole plumbing system.
Danielle Flemming
September 28, 2025 AT 01:09Yo, the whole prosthetic saga is like a roller‑coaster ride through a neon‑lit arcade-thrilling, confusing, and you never know when the lights will go out! If you’re thinking about going for it, make sure you’ve got a solid crew and a game plan. Otherwise, you might end up stuck on level one forever.
Anna Österlund
September 28, 2025 AT 01:25Stop buying into the hype and demand real data.