Every time you pick up a prescription, there’s a good chance the pharmacist handed you a generic version instead of the brand-name drug your doctor wrote on the script. You might not even know it happened. That’s because in 43 states, pharmacists are legally allowed to swap brand drugs for generics without asking you first. This is called presumed consent.
What Presumed Consent Actually Means
Presumed consent doesn’t mean pharmacists can substitute any drug they want. It means they can assume you’re okay with switching to a cheaper, FDA-approved generic version - as long as it’s medically equivalent. The FDA rates these drugs in its Orange Book. If a generic has an “A” rating, it’s considered therapeutically equivalent to the brand. That means it has the same active ingredient, strength, dosage form, and works the same way in your body.
But here’s the catch: you don’t get asked. Not at the counter. Not on the phone. Not even when you pick up your refill. The law assumes you’d rather save money than be consulted. And for most people, that’s fine. Generics cost up to 80% less. The average prescription savings? Around $45 a month. Over a year, that’s nearly $550 back in your pocket.
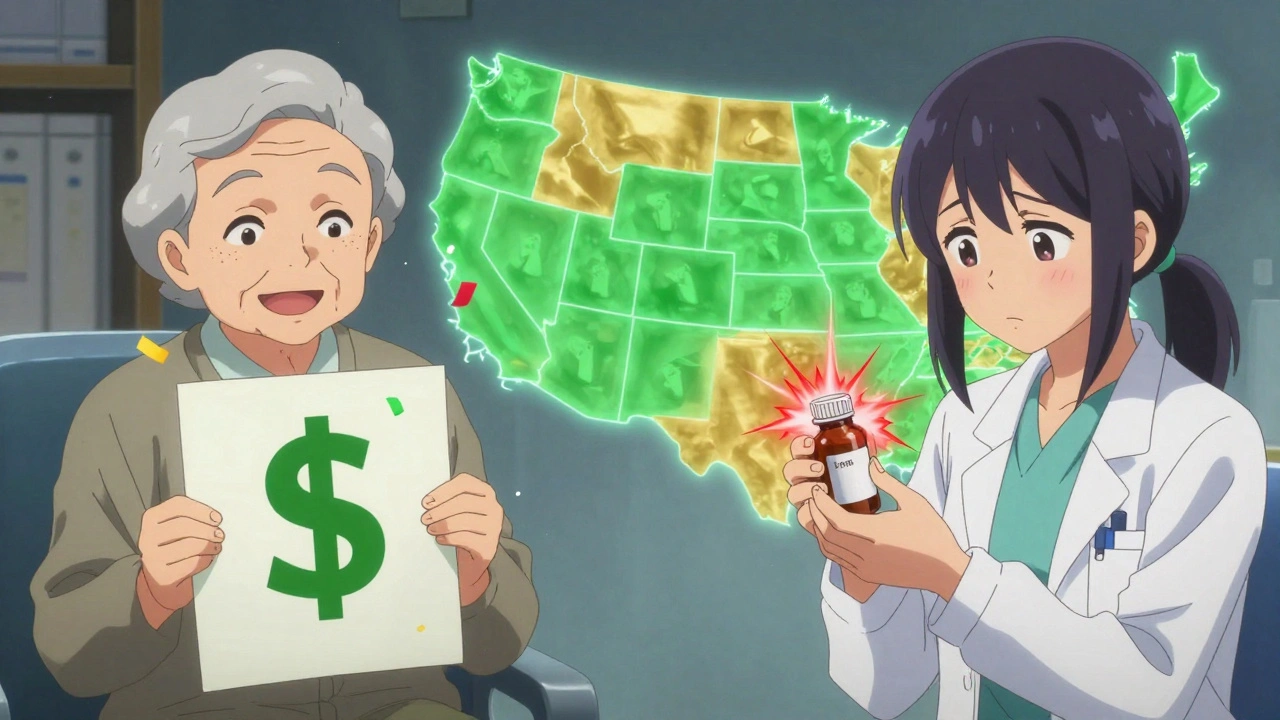
Where the Rules Change - State by State
Not all states play by the same rules. In 19 states, pharmacists are required to substitute generics if they’re available. In 31 others, they can choose to do it - but aren’t forced. And in 7 states plus Washington, D.C., they must ask you first. That’s right: in places like Alaska, Hawaii, and Maine, you have to say yes before the switch happens.
Even in presumed consent states, notification rules vary. Thirty-one states require pharmacists to give you a written or electronic notice after the swap - often tucked inside the pill bottle or sent via text. But in others, you might never know unless you check the label yourself. And if you’re on a drug with a narrow therapeutic index - like warfarin, lithium, or certain epilepsy meds - the rules get stricter. Fifteen states ban automatic substitution for these drugs because even tiny differences in absorption can cause serious side effects.
Why This System Exists - And Why It Works
The whole system was built to save money. Since the 1984 Hatch-Waxman Act, generics have become the backbone of U.S. drug spending. They make up 90% of all prescriptions filled but only 15% of total drug costs. Over the last decade, they’ve saved the healthcare system $1.68 trillion. That’s not a typo. Trillion.
For pharmacies, presumed consent cuts down on delays. Without having to call every patient for approval, a pharmacist can process a prescription 1.7 minutes faster. Multiply that by millions of prescriptions a day, and you’re looking at $2.8 billion saved in labor costs each year. Chain pharmacies use automated systems that flag which drugs can be swapped, reducing errors and speeding up pickup times.
Patients notice the difference, too. On Drugs.com, 68% of comments about generic substitution are positive. People write things like, “Saved me $45 this month,” or “I can finally afford my blood pressure pills.” For seniors on Medicare Part D, the average annual savings from generics is $627. That’s a big deal when you’re living on a fixed income.
The Hidden Risks - When Saving Money Isn’t Safe
But it’s not all smooth sailing. There’s a quiet but growing concern among doctors and patient advocates. For drugs with a narrow therapeutic index - where the difference between a therapeutic dose and a toxic one is razor-thin - switching generics can cause real harm. The American Epilepsy Society documented 178 cases of breakthrough seizures between 2018 and 2022 linked to generic substitutions. In Tennessee, a patient reported his seizure medication stopped working after a switch. He didn’t know it had changed until he saw the pill color was different.
These aren’t rare flukes. The Epilepsy Foundation logged 312 substitution-related adverse events in 2022 alone. Sixty-seven percent of those happened in states without special protections for these high-risk drugs. That’s why 32 states now have special rules for antiepileptics, thyroid meds, blood thinners, and certain psychiatric drugs. Pharmacists in those states must check the patient’s history and sometimes get a doctor’s note before swapping.
Biosimilars - the newer, more complex versions of biologic drugs like Humira or Enbrel - add another layer of confusion. Only 46 states allow automatic substitution for these, and four states - North Carolina, Oklahoma, Pennsylvania, and Texas - ban it entirely. Why? Because biosimilars aren’t exact copies like small-molecule generics. They’re made from living cells, and even small changes in manufacturing can affect how they work. The FDA says they’re interchangeable, but many doctors aren’t convinced.
What Pharmacists Are Really Doing
Most pharmacists support presumed consent - but only if they’re protected. A 2023 survey by the National Community Pharmacists Association found 78% of independent pharmacists in presumed consent states felt confident following the rules. But 41% said special restrictions for high-risk drugs were confusing and time-consuming. One pharmacist in Ohio told Reddit users: “95% of patients don’t notice. The other 5%? They get mad. They think we’re cutting corners.”
That’s why documentation matters. Pharmacists now spend an extra 42 seconds per prescription logging substitutions - more than in states that require consent. They’re not just filling bottles; they’re building legal records. If a patient has a bad reaction, the pharmacy needs proof they followed state law. That’s why tools like the American Pharmacists Association’s online substitution calculator are used by two-thirds of pharmacists. It tells them instantly: “Can I swap this? What’s the notification rule? Is there a restriction?”

What You Can Do - Even If You Don’t Get Asked
You don’t have to sit back and accept whatever you’re handed. Here’s how to take control:
- Check the label. Generic drugs have different names - often the active ingredient plus the manufacturer’s name. If you see “metoprolol succinate” instead of “Toprol-XL,” you’ve been switched.
- Ask your pharmacist. Even in presumed consent states, you have the right to say, “I want the brand.” They can’t refuse unless your insurance blocks it.
- Know your high-risk meds. If you take drugs for epilepsy, thyroid disease, blood thinning, or mental health, ask if your state has special rules. Don’t assume it’s safe.
- Use your insurance app. Many apps show you what you’re being dispensed. Compare the name and manufacturer to your last fill.
- Report changes. If you feel worse after a switch - even slightly - tell your doctor. Document it. You’re not overreacting. You’re protecting your health.
The Future: More Rules, Not Fewer
Right now, the U.S. has 51 different sets of substitution rules - one for each state plus D.C. That’s chaos for pharmacies that operate across state lines. That’s why the Uniform Law Commission proposed a Model State Substitution Act in 2022. It’s gaining traction in 17 states. The goal? Standardize notification, create clear exemptions for high-risk drugs, and make biosimilar rules uniform.
At the same time, pressure is growing to tighten rules for narrow therapeutic index drugs. The American Medical Association has called for federal limits on automatic substitution for these medications. And with biosimilars expected to hit 25% of the biologics market by 2028, the system will need to evolve - fast.
Presumed consent isn’t going away. It’s too cost-effective. But the next five years will see a shift: fewer blanket rules, more targeted protections. The goal isn’t to stop substitution. It’s to make sure it’s safe - for every patient, every time.
Can a pharmacist legally switch my brand-name drug to a generic without asking me?
Yes, in 43 states and Washington, D.C., pharmacists are allowed to substitute a generic version of your prescription without asking for your permission - as long as the generic is rated therapeutically equivalent (an “A” rating) by the FDA. This is called presumed consent. However, they must notify you after the swap in 31 of those states. Seven states plus D.C. require explicit consent before substitution.
Are generic drugs really as safe as brand-name drugs?
For most people, yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and bioavailability as the brand. They must pass strict tests to prove they work the same way. But for drugs with a narrow therapeutic index - like seizure medications, blood thinners, or thyroid pills - even small differences in how the body absorbs the drug can cause problems. That’s why some states restrict substitutions for these drugs.
How do I know if my prescription was switched to a generic?
Check the label. Generic drugs are listed by their active ingredient name (like “metoprolol”) and the manufacturer (like “Sandoz” or “Teva”), not the brand name (like “Toprol-XL”). You’ll also get a printed or digital notice in presumed consent states that require notification. If you’re unsure, ask your pharmacist directly - you have the right to know.
Can I refuse a generic substitution even in a presumed consent state?
Yes. Even in states with presumed consent, you can ask your pharmacist to dispense the brand-name drug. They must honor your request. However, your insurance may not cover the full cost, and you may have to pay more out of pocket. If your doctor wrote “dispense as written” or “no substitution” on the prescription, the pharmacist is legally required to follow that.
Why do some states have special rules for epilepsy or blood pressure drugs?
Drugs with a narrow therapeutic index - such as antiepileptics, warfarin, and lithium - require very precise blood levels to work safely. Even minor differences in how a generic is absorbed can cause side effects or treatment failure. Studies have linked generic switches to breakthrough seizures and dangerous bleeding events. As a result, 32 states now restrict automatic substitution for these medications, requiring pharmacist review or doctor approval before swapping.
Will biosimilars be substituted the same way as generics?
No. Biosimilars are more complex than traditional generics because they’re made from living cells. Only 46 states allow automatic substitution of interchangeable biosimilars, and four states (North Carolina, Oklahoma, Pennsylvania, and Texas) ban it entirely. Many doctors and pharmacists prefer explicit patient consent for these drugs due to their complexity and higher cost. State rules for biosimilars are still evolving, and the FDA’s Purple Book is the official guide for interchangeability.

Akash Sharma
December 2, 2025 AT 19:22I’ve been thinking about this a lot lately, especially since my dad’s on warfarin and we almost didn’t catch the switch last month. It’s wild how the system assumes we’re all okay with saving $45 a month, but for people on narrow therapeutic index drugs, it’s not just about money-it’s about survival. I mean, the FDA says generics are equivalent, but absorption rates can vary by up to 20% between manufacturers, and for someone like my dad, that’s the difference between a clot and a stroke. I wish more pharmacists would proactively flag these cases instead of waiting for patients to notice the pill color changed. And honestly, why aren’t we pushing for mandatory electronic alerts in EHRs? If the system knows what meds you’re on, why can’t it auto-flag when a substitution happens for a high-risk drug? It’s not that I’m against generics-I’m all for cost savings-but there’s a difference between efficiency and negligence.
Justin Hampton
December 4, 2025 AT 18:35So let me get this straight-you’re telling me the government lets pharmacists swap my meds without asking, but I can’t even choose my own toilet paper without a coupon? This is how you know the system’s rigged. They don’t care if you’re stable. They don’t care if you’ve been on the same brand for 12 years. All they care about is squeezing another dime out of your insurance. And don’t even get me started on biosimilars. They’re not generics-they’re Frankenstein drugs made from living cells. Who signed off on this? The same people who thought ‘diet’ soda was a good idea.
Susan Haboustak
December 6, 2025 AT 00:57Let’s be real. The entire premise of presumed consent is a lie. It’s not about saving money-it’s about shifting liability. Pharmacists know full well that patients won’t notice the switch until they start having seizures or bleeding internally. And then what? They point to the label. They point to the state law. They point to the ‘FDA-approved’ sticker. Meanwhile, the patient’s brain is rewiring itself because their epilepsy med was swapped for a cheaper version made in a factory that uses different binders. This isn’t healthcare. It’s corporate risk management disguised as consumer choice. And the fact that 31 states only require notification after the fact? That’s not transparency. That’s cover-your-ass bureaucracy.
Chad Kennedy
December 6, 2025 AT 02:41Siddharth Notani
December 6, 2025 AT 11:59Respectfully, this issue requires nuanced understanding. While generics are statistically safe for 90% of patients, the 10% at risk-particularly those on antiepileptics, anticoagulants, or thyroid agents-deserve mandatory pre-substitution consultation. In India, where I practice pharmacy, we follow a dual-verification protocol: pharmacist + prescriber confirmation for high-risk drugs. Perhaps the U.S. could adopt a tiered system: automatic substitution for low-risk agents, opt-in for high-risk. Technology exists to flag these cases in real time via pharmacy software. Let us leverage it-not ignore it.
Cyndy Gregoria
December 7, 2025 AT 04:00You’re not alone if this freaks you out. I used to be scared too-until I learned how to check my labels and ask questions. Now I always look at the name on the bottle. If it says ‘metoprolol’ instead of ‘Toprol-XL’, I know it’s generic. And if I’m on something like levothyroxine? I tell the pharmacist, ‘I need the brand.’ No questions asked. They respect it. You have rights. Use them. And if you feel weird after a switch? Call your doctor. Don’t wait. Your body tells you things. Listen. You’re not being paranoid. You’re being smart.
Chris Jahmil Ignacio
December 7, 2025 AT 18:48They’re not swapping drugs to save you money. They’re swapping them because the FDA and Big Pharma are in cahoots. Think about it. The same companies that make the brand drugs also make the generics. The FDA gives them the green light because they’re paid off. And now they’re pushing biosimilars-those are just the next step in the plan. You think your Humira is the same? It’s not. The cells are different. The storage conditions are different. The side effects are different. And they don’t want you to know because they’re making billions. This is the New World Order. They control your meds. They control your health. And you’re just sitting there letting them. Wake up.
Paul Corcoran
December 8, 2025 AT 12:46I’ve worked in pharmacies for 20 years, and I’ve seen this play out a thousand times. Most people don’t care. They’re just happy to pay less. But the ones who do care? The ones with epilepsy, thyroid issues, or depression? They’re the ones who come back, trembling, saying ‘I don’t feel right.’ And you know what? We listen. We call the doctor. We switch it back. We log everything. The system’s not perfect, but the pharmacists? We’re trying. We’re not the enemy. We’re the ones reading the labels, checking the Purple Book, and staying up late because we don’t want someone to have a seizure because we swapped a pill without thinking. So if you’re worried? Talk to your pharmacist. We’re here. We care. And we’re not going anywhere.