Running Injury Risk Calculator
Assess Your Injury Risk
Answer these questions to identify your specific injury risks and get personalized prevention strategies.
Whether you’re training for a 5k or a marathon, the goal is the same: keep moving without the pain. The biggest roadblock isn’t lack of motivation-it’s the injuries that pop up when you forget the basics. Below you’ll learn exactly how to prevent running injuries so you can hit your mileage goals with confidence.
Key Takeaways
- Most running injuries stem from weak muscles, poor biomechanics, and inappropriate training loads.
- A structured warm‑up, targeted strength work, and smart gear choices cut injury risk dramatically.
- Listening to your body and tracking stress signals lets you act before a minor ache turns into a sidelining injury.
- Specific prevention strategies differ by injury type; a simple table helps you match the right fix to the right problem.
- Consistent recovery habits-stretching, foam rolling, and adequate sleep-are as crucial as the run itself.
Understanding the Most Common Running Injuries
Common Running Injuries are a set of recurring problems that affect runners of all levels. They typically arise from repetitive stress, muscular imbalances, and sudden spikes in training intensity. Below are the six injuries that show up in over 70% of runner‑related medical visits.
Shin Splints (medial tibial stress syndrome) cause aching along the inner front of the lower leg. They’re often linked to abruptly increasing mileage or running on hard surfaces.
Patellofemoral Pain Syndrome (runner’s knee) produces a dull, grinding pain around the kneecap, especially during hills or stairs. Weak hip abductors and poor knee tracking are the usual culprits.
Achilles Tendinitis feels like a burning or stiffness in the back of the ankle. Tight calf muscles and excessive hill work strain the tendon.
Plantar Fasciitis presents as a sharp heel pain that’s worst with the first steps in the morning. It’s tied to flat feet, high arches, or worn‑out shoes.
Iliotibial (IT) Band Syndrome causes a sharp, localized pain on the outside of the knee that crops up during long runs or downhills. Tight IT band and weak glutes are typical triggers.
Stress Fracture is a tiny crack in a bone (often the metatarsals or tibia) that results from repetitive loading without enough recovery. Early warning signs include persistent, localized bone pain that worsens with activity.
Assess Your Personal Risk Factors
Before you can fix anything, you need to know where you stand. Ask yourself these quick questions:
- Do you have a history of any of the injuries listed above?
- How many days per week do you run, and what’s your average mileage?
- Do you run on concrete, trail, or a treadmill?
- Are you comfortable with basic strength exercises like squats, lunges, and calf raises?
- Do you feel any persistent aches after a run, even if they’re ‘just sore’?
If you answered “yes” to any of the first two, it’s a red flag that you need a more tailored plan.
Build a Prevention‑First Training Routine
Think of injury prevention as a three‑layer cake: warm‑up, strength, and smart progression. Skipping any layer leaves you vulnerable.
1. Dynamic Warm‑Up (5‑10 minutes)
- Leg swings - front‑to‑back and side‑to‑side (10 each leg)
- Walking lunges with a torso twist (12 reps per side)
- High‑knees or butt‑kicks (30 seconds each)
- Ankle circles - clockwise and counter‑clockwise (10 per direction)
Dynamic moves increase blood flow, prime the neuromuscular system, and prime your joints for the repetitive motion of running.
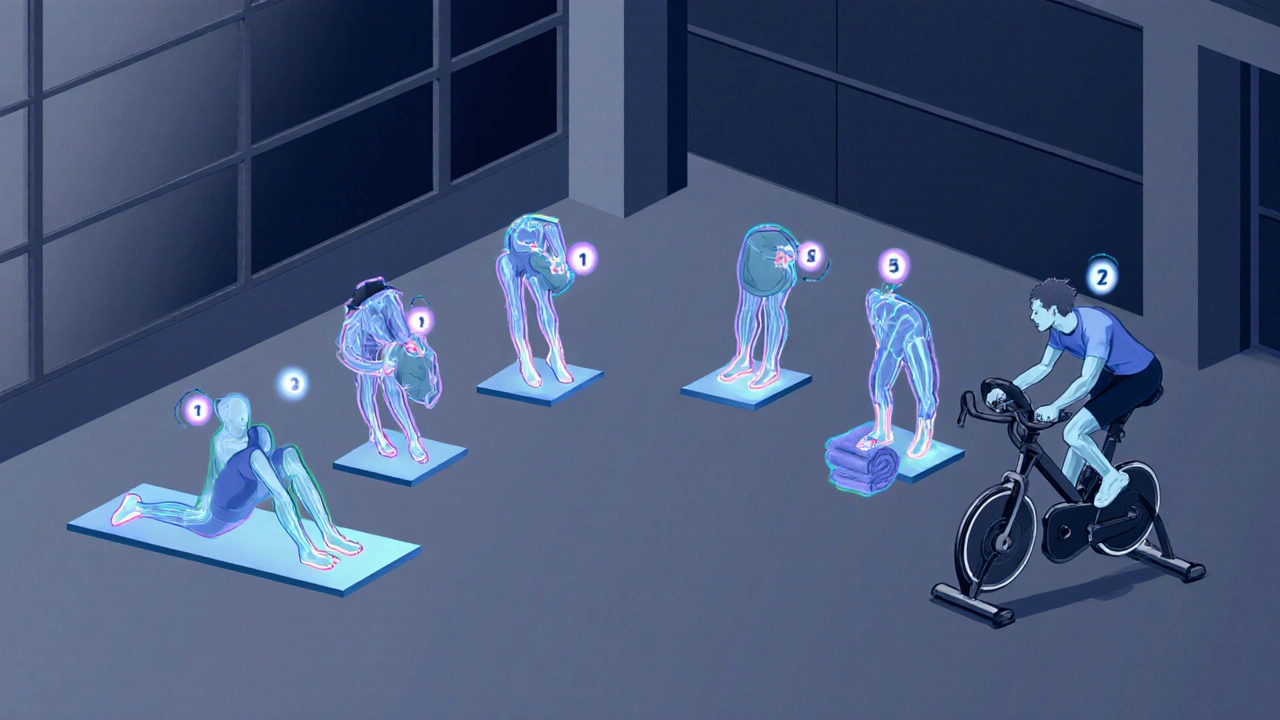
2. Targeted Strength & Mobility (2‑3 sessions per week)
Focus on the muscle groups that support the injuries above.
| Injury | Key Muscles to Strengthen | Example Exercise |
|---|---|---|
| Shin Splints | Tibialis anterior, core stability | Toe raises (3×15) + plank (3×45s) |
| Runner’s Knee | Hip abductors, glute medius | Side‑lying clamshells (3×20 each side) |
| Achilles Tendinitis | Calf (gastrocnemius, soleus) | Eccentric calf raises (3×12 each leg) |
| Plantar Fasciitis | Intrinsic foot muscles, calves | Toe curls with a towel (3×15) |
| IT‑Band Syndrome | Gluteus maximus, hip external rotators | Single‑leg bridge (3×12 each leg) |
| Stress Fracture | Bone density, overall endurance | Low‑impact cross‑training (cycling, swimming) 30min |
Do each exercise with controlled form; quality beats quantity every time.
3. Gradual Load Progression
Follow the 10% rule: increase weekly mileage by no more than 10% and cut back every fourth week (recovery week) by 20‑30%. This lets bone and tendon remodeling keep pace with the stress you’re adding.
Gear, Surface, and Footwear Choices
Running on hard concrete while wearing shoes that are past their 300‑kilometer lifespan is a recipe for trouble.
- Shoes: Replace every 300‑500km. Choose a model that matches your foot strike-neutral cushioning for a mid‑foot strike, stability features for overpronation.
- Orthotics: If you have flat feet or high arches, consider custom or over‑the‑counter insoles that support the arch and reduce heel strain.
- Surface: Mix soft (grass, trail) and firm (track, treadmill) surfaces. Soft surfaces cut impact forces, firm surfaces improve proprioception.
- Clothing: Moisture‑wicking fabrics lower skin friction, decreasing the chance of blisters that can force you to alter gait.
When you combine appropriate gear with a balanced training load, the odds of an injury drop dramatically.

Recovery, Monitoring, and Early Intervention
Running isn’t just the miles you log; it’s also how you treat your body afterward.
- Cool‑down: 5‑minute easy jog or walk, followed by static stretching for calves, quads, hamstrings, and hip flexors.
- Foam Rolling: Spend 1‑2minutes on each major muscle group-especially calves, IT band, and anterior tibialis.
- Sleep: Aim for 7‑9hours per night; growth hormone release during deep sleep is vital for tissue repair.
- Hydration & Nutrition: Adequate protein (1.2‑1.6g/kg body weight) supports muscle recovery; calcium and vitaminD are key for bone health.
- Pain Journal: Log any ache, its location, and intensity. Patterns often reveal overuse before a full‑blown injury appears.
If pain persists beyond a week of diligent recovery, see a sports physiotherapist. Early treatment prevents chronic issues and keeps you on track.
Putting It All Together: A Sample 4‑Week Prevention Plan
- Week1: 3 runs (30min easy, 40min moderate, 20min intervals). Add 2‑day strength routine (table exercises). Finish each run with a 5‑minute cool‑down.
- Week2: Increase total mileage by 8%. Add a hill repeat session (6×30s uphill, jog down). Continue strength work; include extra calf‑eccentric set.
- Week3: Peak week - add 10% mileage. Introduce a 45‑minute cross‑training day (bike or swim). Keep dynamic warm‑up and foam rolling daily.
- Week4 (Recovery): Cut mileage by 25%. Replace one run with a low‑impact activity. Focus on mobility, stretching, and sleep quality.
Adjust the plan based on how your body feels-if a specific ache emerges, swap that day’s run for an extra strength or mobility session.
Frequently Asked Questions
How often should I replace my running shoes?
Most experts recommend swapping them out every 300‑500km (roughly 200‑300miles) or once a year, whichever comes first. Worn‑out midsoles lose cushioning, which raises impact forces on the knees and shins.
Can I still run if I have mild shin splints?
Take a short break (2‑3 days) from hard surfaces, switch to cross‑training, and add tibialis‑anterior strengthening. If pain disappears after a week, you can resume easy runs and gradually build back.
What’s the best surface for a beginner runner?
A synthetic track or a well‑maintained grass field offers a good balance of shock absorption and stability. Avoid very hard concrete until your bones and tendons have adapted.
Is foam rolling actually effective?
Yes. Research from 2023 shows a 15‑20% reduction in delayed‑onset muscle soreness when runners foam‑roll for two minutes per major muscle group after a run.
How can I tell the difference between a stress fracture and a muscle strain?
Stress fractures cause sharp, localized bone pain that worsens with pressure (e.g., jumping) and often persists at rest. Muscle strains feel more like a pulling or throbbing sensation that eases with gentle stretching. If unsure, get an X‑ray or MRI.


aura green
October 12, 2025 AT 16:40Alright, let’s dive into the glorious world of dynamic warm‑ups, because who doesn’t love shaking their limbs like a wet dog before a run? 😊 First, leg swings are the undisputed champion of pre‑run rituals, and you should do ten each direction, no excuses. Then, walking lunges with a gentle torso twist will magically align your spine and hips, twelve reps per side, because alignment is everything. High‑knees or butt‑kicks for thirty seconds each follow, because pretending you’re a hummingbird burns extra calories, right? Ankle circles clockwise and counter‑clockwise, ten each, because rotator cuffs aren’t just for arms. All of this dynamic action pumps blood, primes neuromuscular pathways, and reduces that dreaded shin‑splint feeling that haunts night‑time dreams. Remember, the 10% rule isn’t a law of physics; it’s a polite suggestion from runners who once slipped on concrete. Speaking of concrete, you might want to keep it under a quarter of your mileage, unless you’re auditioning for a role in a slap‑stick comedy. 💪 Shoes should be swapped every 300‑500 km; otherwise, they become death‑traps for your knees and calves. Strength training three times a week, focusing on hip abductors, glutes, and calves, will turn those weak links into steel cables. Foam rolling for a minute or two on calves, IT band, and tibialis anterior is like a spa day for muscles, but cheaper. Sleep, dear runner, is not optional; aim for seven to nine hours, because growth hormone repairs the tiny tears you create on purpose. Hydration and protein intake are your sidekicks; they keep tissues happy and bones dense. Keep a pain journal; it’s the detective that catches injuries before they become headlines. If any ache persists beyond a week, see a physio-you’re not a martyr, you’re a human. Finally, remember that recovery isn’t laziness, it’s strategic planning for the next epic run. 🌟
Sriram K
October 13, 2025 AT 05:10Adding a solid strength routine can dramatically lower the risk of those classic running injuries. Focus on the hip abductors, glutes, and calf muscles with exercises like side‑lying clamshells, single‑leg bridges, and eccentric calf raises. Aim for 3 sets of 12‑15 reps, two to three times a week, and progressively increase the load as you get comfortable. Consistency is key-missing a session repeatedly negates the benefits. Also, don’t forget core work; a stable core supports proper biomechanics and reduces stress on the knees and shins. Balance these sessions with your running schedule, ensuring you have at least a day of rest or low‑impact activity between hard runs and strength days. This approach helps tissues adapt, minimizing overuse injuries.
Deborah Summerfelt
October 13, 2025 AT 17:40So the ‘10% rule’ is basically a myth invented by people who never push themselves past a comfortable couch. If you’re trying to get faster, you need to break the comfort barrier, not hide behind arbitrary percentages. Real progress comes from occasional spikes in mileage, followed by strategic cut‑backs, not a sterile, linear climb. Besides, the body adapts to stress in unpredictable ways; you can handle a sudden 15% jump if you’ve built a solid base. The key is listening to your own signals, not a one‑size‑fits‑all rulebook. And let’s be honest, most runners who stick to the rule end up a decade older with a “steady” pace, never truly testing their limits.
Maud Pauwels
October 14, 2025 AT 06:26great points about strength work and recovery get proper rest and vary surfaces for lower impact
Scott Richardson
October 14, 2025 AT 19:13American runners should be proud of our miles but also aware that too many concrete routes can ruin ankles. Keep shoes fresh and stay on softer trails when you can for a stronger nation of runners.
Laurie Princiotto
October 15, 2025 AT 08:00Whoa there, patriot! You sound like you’re defending a flag while ignoring the actual data. Concrete isn’t just a "evil" surface; it’s a reality for most city dwellers. If you can’t afford trails, upgrade your shoes more often and add strength drills, period.
Justin Atkins
October 15, 2025 AT 20:46From a biomechanical perspective, bone remodeling follows Wolff’s law, which dictates that bone density adapts to the magnitude and direction of mechanical loads. When runners increase their weekly mileage, cortical thickness in the tibia and metatarsals augments, provided the stress remains within physiological limits. However, excessive repetitive stress without adequate recovery precipitates micro‑fractures, which coalesce into stress fractures if unchecked. Therefore, the gradual progression of training load is not merely a precautionary whim; it is a cornerstone of osteogenic adaptation. Incorporating low‑impact cross‑training such as cycling or swimming allows for cardiovascular maintenance while mitigating excessive compressive forces on the lower extremities. Moreover, proper nutrition-adequate calcium, vitamin D, and protein-facilitates mineralization and repair processes. In essence, the synergy of progressive overload, strategic rest, and nutritional support cultivates resilient skeletal structures capable of withstanding the rigors of distance running.
June Wx
October 16, 2025 AT 09:33Sure, you sound fancy, but most of us just want to run without breaking a bone. So yeah, mix in a bike day, eat your milk, and don’t do 40 miles every week if you’re not ready. Simple.
kristina b
October 16, 2025 AT 22:20In the grand theater of human endeavor, the quest for injury‑free endurance runs assumes a metaphysical significance that transcends the mere mechanics of musculature and bone. Consider the runner as a pilgrim traversing the undulating terrain of existence; each stride becomes a stanza in a poem of perseverance, each breath a whispered prayer to the cosmos. The dynamic warm‑up, far from a perfunctory ritual, serves as an invocation, summoning the latent kinetic energy within the fibers of the lower limbs. Leg swings, with their sinusoidal motion, echo the pendulum of time, reminding the athlete that motion is perpetual and stagnation fatal. Walking lunges, intertwined with torso twists, enact a delicate ballet of torsional synergy, harmonizing the sagittal and transverse planes in a dance of equilibrium. High‑knees and butt‑kicks, those theatrical gestures, conjure the spirit of youthful exuberance, reawakening neural pathways that dormant adulthood often neglects. Ankle circles, drawn in clockwise and counter‑clockwise motions, symbolize the cyclical nature of life, reinforcing proprioceptive acuity. These preparatory movements collectively sculpt the neuromuscular orchestra, ensuring that each subsequent cadence resonates with precision.
Strength training, then, is not a mere adjunct but the very foundation upon which the edifice of resilience is built. By engaging the hip abductors, gluteal medius, and calf complex through targeted exercises-clamshells, single‑leg bridges, eccentric calf raises-the runner fortifies the pillars that bear the weight of relentless impact. This fortification is akin to reinforcing a cathedral’s arches; without it, collapse is inevitable.
The selection of footwear, a seemingly pedestrian concern, in truth reflects a philosophical commitment to stewardship of the self. Replacing shoes at the 300‑500 km threshold is an act of reverence toward one’s own corporeal vessel, acknowledging that worn midsoles betray the runner’s noble intentions. Orthotics, when warranted, become the subtle artisans, reshaping the foot’s architecture to align with the individual’s inherent gait patterns.
Recovery, that oft‑neglected sanctuary, demands solemn devotion. Sleep, the nocturnal alchemy, transmutes cellular fatigue into regenerative vigor, a process orchestrated by the symphony of growth hormone and cortisol. Nutrition, the sustenance of the soul, must furnish adequate protein, calcium, and vitamin D, lest the body’s scaffolding erode under the strain of repeated loading.
Thus, the runner, armed with knowledge, embraces a holistic regimen: warm‑up as rite, strength as foundation, footwear as covenant, and recovery as sacrosanct ritual. In doing so, the specter of shin splints, runner’s knee, Achilles tendinitis, plantar fasciitis, IT‑band syndrome, and stress fractures recedes, yielding to the luminous horizon of untethered, injury‑free motion.
Ida Sakina
October 17, 2025 AT 11:06The discourse on injury mitigation is commendable and aligns with ethical imperatives to safeguard athletes. It is imperative to adopt the prescribed protocols diligently.
Amreesh Tyagi
October 17, 2025 AT 23:53i think the whole shoe mileage thing is exaggerated but ok
Brianna Valido
October 18, 2025 AT 12:40Totally agree! 🙂 Keeping shoes fresh and listening to your body is the way to go! 🌟
Caitlin Downing
October 19, 2025 AT 01:26hey guys i love the vibe here but just wanna point out that my coach always says using “dynamic warm‑up” isn’t just a buzz‑word its real work for the muscles and it does wonders for form
Robert Jaskowiak
October 19, 2025 AT 14:13Wow, a whole paragraph about warm‑ups? Guess we’re all set to become Olympic sprinters now. 🙄
Julia Gonchar
October 20, 2025 AT 03:00Just a heads‑up: if you keep ignoring the 10% rule, you’ll likely end up with a stress fracture. It’s not a myth, it’s backed by research.
Annie Crumbaugh
October 20, 2025 AT 15:46Interesting read.
Vic Harry
October 21, 2025 AT 04:33Run fast stay strong and don’t be lazy about shoes