If your child swallows the wrong medication, time is the most critical factor. Every second counts. The difference between a quick recovery and a life-threatening emergency often comes down to what you do in the first five minutes. This isn’t about panic-it’s about knowing exactly what to do, and what not to do.
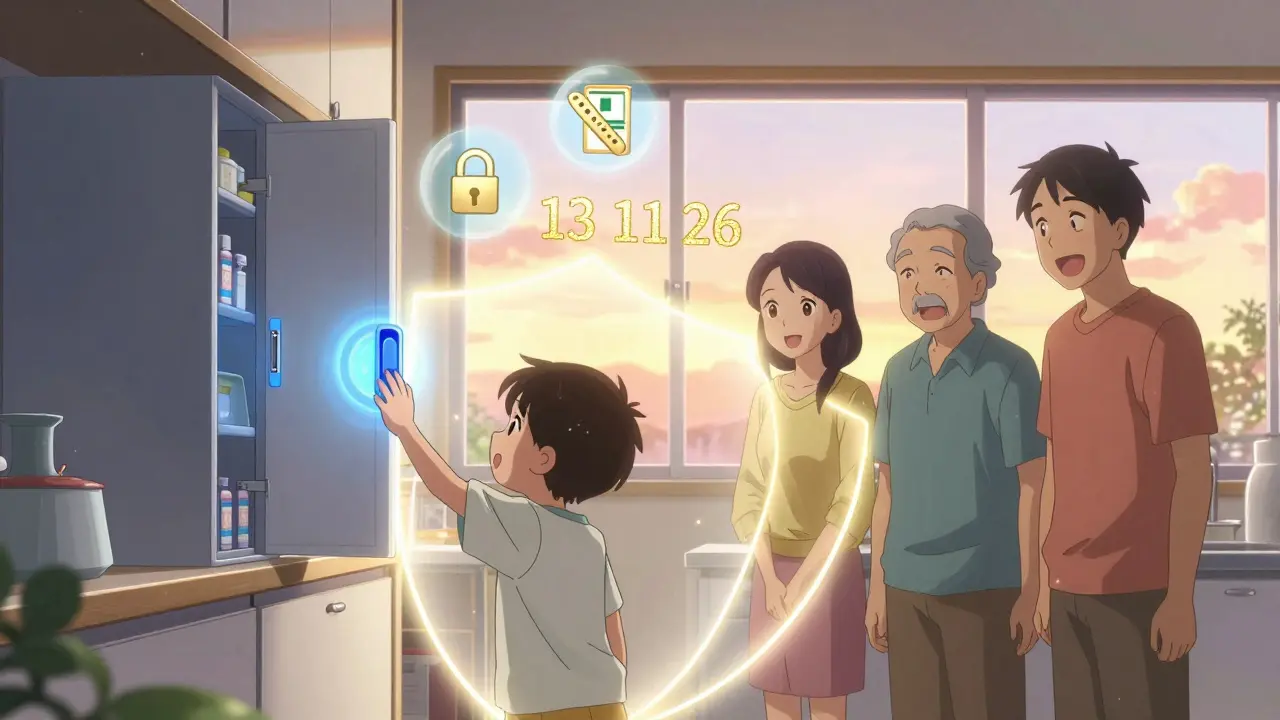
Call Poison Control Immediately
The very first thing you must do is call Poison Control. In Australia, that’s 13 11 26. Don’t wait. Don’t try to figure out if it’s serious. Don’t Google symptoms. Call now. Poison Control specialists are trained to ask the right questions in seconds: What was swallowed? How much? When? How old is the child? They’ll tell you whether to wait at home or rush to the hospital. This isn’t a suggestion-it’s the standard of care. According to the Australian Poison Information Centre, families who call Poison Control first are 43% less likely to end up in the hospital. In the U.S., the same data holds true. These centers don’t just give advice-they guide you through real-time decisions that save lives.Remove Any Remaining Medication
While you’re on the phone with Poison Control, gently remove any leftover pills, liquid, or patches from your child’s mouth. Use your fingers. Don’t force it. If a patch is stuck to their skin, peel it off carefully. If it’s a chewable tablet, check their gums and tongue. Medication patches, especially those for pain or nicotine, can stick to the roof of the mouth or inside the cheeks. They continue releasing drugs for hours. Missing one could mean a delayed reaction. Don’t try to make your child spit it out. Don’t give them water or milk to flush it down. Don’t induce vomiting. That’s the biggest mistake parents make.Never Induce Vomiting
You might have heard older advice to give syrup of ipecac. That’s outdated. Since 2004, every major medical group-including the American Academy of Pediatrics and the Australian Therapeutic Goods Administration-has banned it. Why? Vomiting doesn’t remove enough of the drug. And it can make things worse. If the substance is caustic, like bleach or cleaning products, vomiting can burn the throat again on the way up. If it’s a pill, vomiting increases the risk of choking or aspiration pneumonia. In 7% of cases where parents tried to make their child vomit, they ended up in the hospital for lung complications. Let the experts handle it. Poison Control will tell you if activated charcoal is needed. That’s given in hospitals under supervision. It’s not something you give at home.
Watch for These Warning Signs
Some reactions happen fast. Others creep in over hours. Watch for these red flags:- Difficulty breathing or stopped breathing
- Losing consciousness, even briefly
- Seizures or unusual shaking
- Pupils that are unusually large or tiny
- Extreme drowsiness lasting more than 20 minutes
- Excessive drooling or foaming at the mouth
- Persistent vomiting or nausea
- Fast, slow, or irregular heartbeat
What Happens at the Hospital
If you’re told to go to the ER, bring the medication container-even if it’s empty. The label has the active ingredients, strength, and expiration date. That’s critical. If it’s a liquid, bring the measuring cup. If it’s a patch, bring the wrapper. At the hospital, they’ll monitor your child’s vital signs every 15 minutes for the first hour. If it’s a heart medication, they’ll run an ECG. If it’s a painkiller like acetaminophen, they’ll check liver enzymes. If it’s a diabetes pill (sulfonylurea), they’ll test blood sugar every 30 minutes-low blood sugar can cause seizures or coma. They might give:- Naloxone for opioid overdoses (like codeine or tramadol)
- Octreotide for insulin-like pills that crash blood sugar
- Sodium bicarbonate for antidepressants that affect heart rhythm
- Activated charcoal if it’s been less than an hour since ingestion
Why Some Cases Are Worse Than Others
Not all medications are equal. Some are deadly in tiny amounts.- Acetaminophen (paracetamol): One adult tablet can be toxic to a toddler. It’s the leading cause of pediatric poisoning deaths.
- Beta-blockers (like metoprolol): Used for high blood pressure. A single pill can stop a child’s heart.
- Calcium channel blockers (like amlodipine): A 5 mg tablet can cause dangerous drops in heart rate and blood pressure.
- Antidepressants (like sertraline): Can cause seizures and serotonin syndrome.
- Insulin or diabetes pills: Can cause life-threatening low blood sugar within 30 minutes.
How to Prevent This From Happening Again
The best emergency plan is no emergency at all.- Lock it up. Use a locked cabinet, not just a high shelf. Most children can climb, open drawers, or pull down cabinets by age 2.
- Use child-resistant caps. Not all are equal. Look for those with two-step locks-press and turn. Since 2022, Australian regulations require flow restrictors on liquid medications to reduce accidental overdose volume by 58%.
- Never leave meds on counters. Even for a minute. That’s when it happens.
- Use smart pill boxes. Devices like Hero Health alert you if a dose is missed and lock the compartment. They’re $89.99/month, but in homes with young kids, they’ve reduced accidental access by 73%.
- Dispose of old meds properly. Don’t flush them. Take them to a pharmacy with a take-back program. Many Australian pharmacies offer free disposal.
What Parents Get Wrong
Most parents think they’ll know what to do. But studies show 61% of Australian families can’t recall the Poison Control number. That’s why the Australian Poisons Information Centre runs the “Know the Number” campaign. Write it down. Save it in your phone. Stick it on the fridge. Teach your partner, your babysitter, your grandparents. Another myth: “It was just one pill.” One pill can be enough. One chewable antihistamine can cause hallucinations. One blood pressure pill can stop a heart. Don’t downplay it. And don’t rely on apps or online tools alone. The webPOISONCONTROL tool is accurate 94% of the time-but it’s not a replacement for a live expert. Use it to prepare, not to delay.Final Reminder
You’re not alone. This happens more than you think. In Australia, over 2,000 children under 5 are treated for accidental medication ingestion every year. But most of these cases have good outcomes-because parents acted fast. Call Poison Control first. Remove what’s left. Don’t make them throw up. Watch for symptoms. Get to the hospital if needed. And lock it all up tomorrow.It’s not about being perfect. It’s about being ready.


Ian Ring
January 5, 2026 AT 00:07Just saved this to my phone under 'EMERGENCY'-and told my wife to do the same. I never thought I'd need it, but now I'm scared I didn't do it sooner. Thanks for the clarity. 😅
erica yabut
January 5, 2026 AT 17:49Oh, so you're telling me the only thing standing between a toddler and a coffin is a phone number? How quaint. Meanwhile, in Sweden, they've had mandatory childproof packaging since the '90s-and not a single parent has to Google 'what to do if my kid ate my Adderall' because, shocker, we don't leave psychoactive pharmaceuticals in the same drawer as gummy vitamins. But sure, let's keep treating poison control like a hotline for negligent parenting.
Tru Vista
January 7, 2026 AT 03:11Acetaminophen toxic at 150mg/kg? Yeah but most kids swallow 10 tabs so it's like 1.5g max. Liver tox starts at 7.5g. You're exaggerating. Also, ipecac is fine if you're fast. WHO still says it's okay in low-resource settings. Also, why no mention of activated charcoal dosing? Lazy post.
Vincent Sunio
January 7, 2026 AT 04:43The assertion that 'time is the most critical factor' is both trivial and imprecise. Critical to what? Survival? Neurological outcome? The distinction between immediate intervention and delayed care is not adequately contextualized within pharmacokinetic thresholds. Moreover, the reliance on Poison Control as a first-line triage mechanism presupposes ubiquitous access to telecommunication infrastructure-an assumption that fails under socioeconomic scrutiny. A more rigorous analysis would account for systemic disparities in emergency response equity.
Haley Parizo
January 7, 2026 AT 12:54My cousin’s kid swallowed a blood pressure pill. She called Poison Control. They told her to stay calm, remove the remaining tablet, and drive straight to the ER. They got there in 12 minutes. Kid was fine by morning. No vomiting. No panic. Just action. That’s the difference between fear and preparation. This isn’t about being perfect-it’s about being present. And if you think your child is safe because you 'keep meds high up,' you’re already one climbing expedition away from a nightmare.
Shruti Badhwar
January 7, 2026 AT 13:32As a nurse in Mumbai, I’ve seen this too often. Parents give water to 'dilute' the pill. Or they rush to the hospital without the bottle. We spend 20 minutes trying to figure out what was ingested. Please-bring the container. Even if it’s empty. The label saves lives. Also, lock it. Not just 'out of reach.' Locked. With a key. Not a child-proof cap that a 3-year-old can open after watching YouTube tutorials.
Liam Tanner
January 9, 2026 AT 08:59Good stuff. I’ve been teaching this to my sister-in-law who babysits her grandkids. She didn’t even know Poison Control had a live chat option now. I showed her the app. She’s gonna print the number and stick it on the fridge next to the microwave. Simple. But so many people miss this. Thanks for the reminder.
Palesa Makuru
January 9, 2026 AT 10:51Wow, so we’re supposed to trust Poison Control over our own instincts? I mean, what if they’re wrong? What if they’re just reading from a script? I read online that some of these centers are understaffed and use AI chatbots now. And what about the parents who don’t speak English? This whole thing feels like a corporate PR campaign disguised as public health. Also, why are you blaming parents? The pharmaceutical industry makes billions off this fear.
Hank Pannell
January 11, 2026 AT 09:25There’s a deeper philosophical layer here: the erosion of embodied parental intuition in favor of institutionalized protocols. We’ve outsourced our survival instincts to centralized systems-Poison Control, Google, Alexa-because we’re too busy, too anxious, too disconnected from the rhythms of the body. But when the system fails-and it will-the child doesn’t care about your algorithm. They care about your hands. Your voice. Your presence. Locking up meds is good. But being present? That’s the real prevention.
veronica guillen giles
January 11, 2026 AT 23:20Oh sweetie, you really think a locked cabinet is gonna stop a 2-year-old who’s been watching Peppa Pig for 12 hours straight? They’ll climb the fridge, knock over the laundry basket, and find the pill bottle in your husband’s gym bag. This isn’t a parenting tip-it’s a fantasy. But hey, at least you got the emoji right. 🤦♀️
Neela Sharma
January 13, 2026 AT 20:53One pill. One second. One decision. That’s all it takes. I held my daughter while she seized because I thought 'it’s just a cough syrup.' I didn’t call Poison Control-I called my mom. She told me to wait. I waited 17 minutes. We lost 12 hours of brain time. Don’t wait. Don’t think. Don’t Google. Call. Now. Your child doesn’t need a lecture. They need you to move.
innocent massawe
January 15, 2026 AT 14:01Thank you for this. My brother’s son did this last year. He swallowed a melatonin gummy-thought it was candy. They called Poison Control. They said stay calm. Watch breathing. No vomiting. They went to ER. Kid was fine. Now my whole family has the number saved. Simple. But powerful. 🙏
JUNE OHM
January 17, 2026 AT 10:54POISON CONTROL IS A GOVERNMENT TRAP. They’re just trying to get you to the hospital so they can charge you $20,000 and give your kid a 'toxicology report' that gets sold to Big Pharma. I’ve seen the videos. The pills are all laced with microchips. Call your local naturopath. Use activated charcoal from the health store. And for god’s sake, don’t let the state tell you how to parent. 🚩💊