Most people think if a drug makes them feel bad, it’s an allergy. But that’s not always true-and getting it wrong can be dangerous. You might say you’re allergic to penicillin because you got sick after taking it, but chances are, you didn’t have an allergy at all. You had a side effect. And if you keep believing it’s an allergy, you could end up on stronger, more expensive, and riskier antibiotics-just because you misunderstood what happened to your body.
What’s the Real Difference?
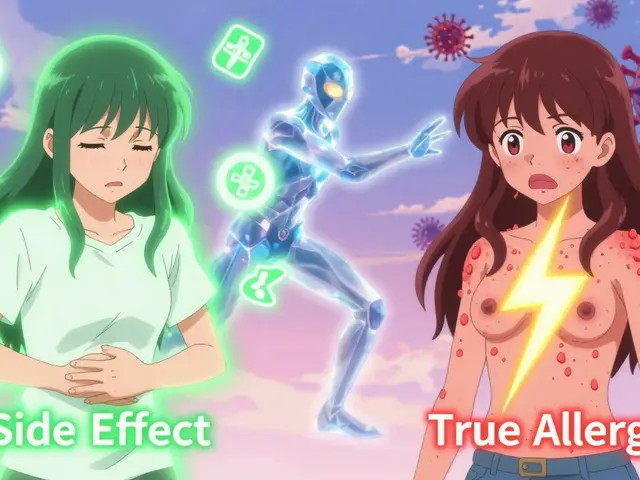
A side effect is what happens when a drug does something it’s not supposed to do-usually because of how it works in your body. For example, antibiotics like amoxicillin can upset your stomach because they kill off good bacteria along with bad ones. That’s not your immune system attacking the drug. It’s just chemistry. Nausea, dizziness, headaches, and dry mouth are all classic side effects. They’re listed in the patient info sheet for a reason: they’re expected, predictable, and usually mild. A true drug allergy is different. It’s your immune system mistaking the drug for a threat-like a virus or pollen-and launching a full attack. That’s why allergic reactions can get worse every time you take the drug. Your body remembers it. And next time, it doesn’t just make you queasy-it might break out in hives, swell your throat, or drop your blood pressure. That’s anaphylaxis. It’s life-threatening. And it’s not common. Only about 5 to 10% of all bad reactions to drugs are real allergies.Timing Tells the Story
When did the reaction happen? That’s your first clue. If you felt sick within minutes to an hour after taking the pill? That’s a red flag for allergy. Hives, itching, swelling of the lips or tongue, wheezing, or trouble breathing? Those are immune signals. The body releases histamine fast-like a smoke alarm going off. That’s IgE-mediated allergy, the most dangerous kind. But if you started feeling nauseous or dizzy 12 hours later? Or got a rash three days after starting the medicine? That’s more likely a side effect-or a delayed reaction that still needs attention. Delayed rashes can be allergic too, like the kind you get with sulfa drugs or some seizure medications. But they’re not the same as the sudden, full-body reaction you get with penicillin or peanuts.One System or Many?
Side effects usually stick to one area. Stomach? That’s nausea. Head? That’s a headache. Drowsy? That’s sedation. Simple. Allergies? They rarely stay in one place. If you get a rash and your throat swells and you feel dizzy? That’s multiple systems reacting. That’s the immune system in overdrive. A 2023 analysis of 10,000 patient records found that 87% of true drug allergies involved at least two body systems. Only 22% of side effects did. Think of it like this: a side effect is a glitch in the software. An allergy is a hacker breaking in.
Common Misunderstandings
The biggest mistake? Confusing stomach upset with an allergy. A 2022 study in JAMA Internal Medicine found that 68% of people who thought they were allergic to penicillin were actually just nauseous. That’s not an allergy. That’s a side effect. And yet, those people avoid penicillin for life-often switching to broader antibiotics that are more expensive, less effective, and more likely to cause dangerous infections like C. diff. Another myth: “I got a rash once, so I’m allergic.” Not always. Some rashes are just a reaction to the drug’s chemical structure-not your immune system. The FDA’s 2023 guidelines now require drug labels to clearly separate “side effects” from “allergic reactions.” That’s because too many people are scared of drugs they could safely take.What About Penicillin?
Penicillin is the classic example. About 10% of Americans say they’re allergic to it. But when they’re tested-through skin tests or supervised challenges-90 to 95% turn out to be fine. That’s not a fluke. It’s a pattern. The Penicillin ImmunoCAP test, approved by the FDA in 2023, finds specific IgE antibodies with 97% accuracy. If you’re told you’re allergic but never got tested, you’re probably not. And you’re missing out on the safest, cheapest, most effective antibiotic for many infections. Hospitals are catching on. In 2020, only 15% of U.S. hospitals had formal programs to retest people who claimed penicillin allergies. By 2023, that number jumped to 42%. Mayo Clinic’s program successfully de-labeled 92% of low-risk patients. No one got hurt. And their treatment got better.What Should You Do?
If you think you have a drug allergy, ask yourself:- Did the reaction happen within an hour?
- Did you get hives, swelling, trouble breathing, or dizziness?
- Did more than one part of your body react?
- Did it get worse the next time you took the drug?

Why This Matters
Getting this right isn’t just about comfort. It’s about safety and cost. The CDC estimates that mislabeling penicillin allergies adds $1.1 billion to U.S. healthcare costs every year. Patients with false allergy labels have 30% longer hospital stays. They’re 69% more likely to get C. diff infections. And they’re often given antibiotics that are harder on the body and worse for the planet-because they’re overused. There’s also a personal cost. You might avoid life-saving meds because you think you’re allergic. You might get sicker because you’re on a less effective drug. You might even die because no one realized your reaction wasn’t an allergy.What’s Changing Now?
The medical world is waking up. In 2024, the American College of Allergy, Asthma, and Immunology will officially update its guidelines to use three clear terms:- Allergy = immune system reaction (IgE or T-cell)
- Intolerance = unpleasant but non-immune reaction (like nausea or dizziness)
- Side effect = expected, dose-related effect (like sleepiness from antihistamines)
Bottom Line
You don’t need to be a doctor to tell the difference. Look at the symptoms. Look at the timing. Look at how many body systems were involved. If it was just nausea or a headache? Probably not an allergy. If you broke out in hives, swelled up, or couldn’t breathe? That’s serious-and you need to get it checked. Don’t let a misunderstanding keep you from the best treatment. If you’ve been avoiding a drug because you thought you were allergic, ask your doctor about testing. You might be surprised-and your health will thank you.Can you outgrow a drug allergy?
Yes, especially with penicillin. About 80% of people who had a true penicillin allergy as a child lose the sensitivity after 10 years. That’s why retesting is so important-even if you were told you were allergic decades ago, you might be fine now. Skin tests or supervised challenges can confirm whether your immune system still reacts.
Is a rash always a sign of a drug allergy?
No. Many rashes from drugs are not allergic. Viral infections, heat, or even the drug’s chemical irritation can cause rashes. A true allergic rash is usually itchy, raised, and appears quickly after taking the drug. Delayed rashes (like those from sulfa or allopurinol) can be serious, but they’re still immune-mediated. If you’re unsure, get it checked-don’t assume it’s harmless.
Can you have an allergic reaction the first time you take a drug?
Rarely. The immune system needs to be exposed first to recognize the drug as a threat. So true IgE-mediated allergies usually happen on the second or later exposure. But sometimes, cross-reactivity with similar molecules (like in foods or environmental allergens) can cause a first-time reaction. Still, if you react the very first time, it’s more likely a side effect or a non-allergic hypersensitivity.
What if I had a reaction but didn’t go to the doctor?
Document it now. Write down the drug name, the dose, the symptoms, and when they started. Even if you didn’t see a doctor at the time, this record helps future providers decide if it was an allergy or side effect. Many people forget details after years. The sooner you record it, the better.
Are over-the-counter drugs like ibuprofen or aspirin common allergy triggers?
They’re more likely to cause side effects than true allergies. Nausea, stomach upset, or headaches from NSAIDs are common. A true allergy to aspirin or ibuprofen is rare and usually involves breathing problems, hives, or swelling-not just stomach pain. If you’ve had a reaction with breathing trouble, see an allergist. If it’s just an upset stomach, it’s probably not an allergy.
Can I take another drug in the same class if I’m allergic to one?
Sometimes, but not always. Penicillin and amoxicillin are in the same family, so if you’re allergic to one, you’re likely allergic to the other. But not all drug classes work that way. For example, someone allergic to one sulfa drug might tolerate another. Never assume. Always talk to your doctor or allergist before trying a related drug.

Lynsey Tyson
December 19, 2025 AT 17:59I used to think I was allergic to penicillin because I got a rash after taking it in high school. Turns out it was just a viral rash that happened to coincide with the antibiotic. Got tested last year and now I can take it without fear. My doctor said I was one of the 90% who got mislabeled. Life’s easier now.
Also, side effects are way more common than people realize. I get dizzy on blood pressure meds? Not an allergy. Just my body adjusting. Stop panicking and talk to your doc.
Edington Renwick
December 21, 2025 AT 04:41Wow. Just wow. So now we’re supposed to trust doctors who can’t even tell the difference between a stomach ache and anaphylaxis? This article reads like a pharmaceutical lobby pamphlet.
Let me guess - next they’ll say vaccines are just ‘side effects’ too. Wake up people. The system is lying to you to push cheaper drugs. And you’re eating it up.
Allison Pannabekcer
December 21, 2025 AT 16:43My grandma was told she was allergic to penicillin in the 60s. She never took it again. At 82, she got a severe UTI and ended up in the hospital on a super-strong antibiotic that gave her diarrhea for weeks. Turns out she never had an allergy - just nausea. They did a skin test and she cried because she realized she’d been avoiding safe meds for 60 years.
Don’t let fear make your health worse. If you’ve been avoiding a drug because of a bad reaction years ago - get tested. It’s simple. It’s safe. And it might save your life.
Sarah McQuillan
December 22, 2025 AT 00:00Oh please. You think this is some big revelation? Everyone knows side effects aren’t allergies. This is like writing an article titled ‘Water is Wet.’
Also, why are we trusting the FDA? They approved OxyContin. They approved Vioxx. They approved 37 drugs that got pulled later. You really think they’re on our side? This is just corporate spin dressed up as medicine.
Aboobakar Muhammedali
December 22, 2025 AT 17:28I took amoxicillin once and got a rash on my chest. I thought it was allergy. I avoided all antibiotics for years. Last year I got pneumonia. My doctor said ‘try amoxicillin again - you’re not allergic.’ I did. Nothing happened. No rash. No problem.
Turns out it was just my skin reacting to the heat that day. Not the drug. I feel stupid now. But also relieved.
Don’t assume. Get checked. It’s not hard.
anthony funes gomez
December 24, 2025 AT 11:15There's a critical epistemological distinction here: the phenomenological experience of adverse reaction ≠ the immunological mechanism of hypersensitivity. The conflation of these constructs is not merely semantic-it’s iatrogenic.
When patients self-diagnose ‘allergy’ based on non-IgE-mediated events (e.g., GI distress, transient dizziness), they activate a cascade of therapeutic substitution that increases microbial resistance, healthcare expenditure, and morbidity. The data is unequivocal. Yet the lay public persists in linguistic sloppiness. We need better public health literacy. Not just better labeling.
Laura Hamill
December 25, 2025 AT 08:26They’re lying. All of them. The FDA, the doctors, the hospitals. Why do you think they want you to think it’s ‘just a side effect’? So they can keep giving you the same poison. Penicillin is laced with fluoride. They’ve been doing this since the 1950s. You think your rash is from the drug? Nah. It’s from the chemicals they add to make you dependent on stronger meds.
Don’t trust the system. Go herbal. Or don’t take anything at all. 🤔👁️
Alana Koerts
December 26, 2025 AT 04:53So what? You told me something I already knew. And you didn’t even mention the fact that most ‘allergy tests’ are unreliable. Skin tests have a 30% false positive rate. Oral challenges can be dangerous. You’re just replacing one myth with another.
Also, ‘side effect’ is just a euphemism for ‘we knew this would happen but didn’t care.’
Thanks for the article. Now I know exactly nothing new.
pascal pantel
December 26, 2025 AT 10:13Let’s cut the fluff. The real issue isn’t terminology. It’s liability. Doctors don’t want to be sued if someone has a reaction. So they label everything ‘allergy’ and move on. Patients don’t want to risk death, so they accept the label. The system is broken. The science? Fine. The practice? Toxic.
And yes - I’ve seen patients die because they were on vancomycin instead of penicillin. Because someone checked a box they didn’t understand.
Gloria Parraz
December 27, 2025 AT 17:02This is so important. I’m a nurse and I’ve seen this over and over. People avoid life-saving meds because of a stomach ache they had 20 years ago. Please, if you’ve ever felt weird after a drug - write it down. Don’t just say ‘allergic.’ Say what happened. When. How long it lasted.
And if you’re scared? Talk to your doctor. Not Google. Not Reddit. Your doctor. They’re there to help.
You’re not alone. And you’re not crazy. But you might be misinformed.
Sahil jassy
December 28, 2025 AT 00:06I had a rash after amoxicillin in college. Thought I was allergic. Never took it again. Last year I got strep throat. My doc said ‘try it.’ I did. No rash. No problem.
Turns out I had a virus that day. The drug had nothing to do with it. I feel so dumb now but also so relieved. If you think you’re allergic - get tested. It’s easy. It’s free in many places. Don’t live in fear.
Thank you for this post. I needed to hear it.
Nicole Rutherford
December 29, 2025 AT 06:32Of course you’re allergic. You just don’t know it yet. They’re all lying. The CDC, the FDA, your doctor - they’re all paid by Big Pharma. That’s why they want you to think it’s ‘just a side effect.’ So they can keep selling you dangerous drugs. You think penicillin is safe? It’s been linked to autism, depression, and infertility. And they’re hiding it.
Don’t be fooled. Your body knows. That rash? That nausea? That’s your soul screaming.