Penicillin Allergy: What It Is, How It Affects You, and What to Do
When someone says they have a penicillin allergy, an immune system reaction to penicillin antibiotics that can range from mild rash to life-threatening anaphylaxis. Also known as beta-lactam allergy, it’s one of the most commonly reported drug allergies in the U.S.—but up to 90% of people who believe they have it don’t actually react when tested. Many people outgrow it over time, and some were never allergic to begin with—maybe they had a viral rash while taking amoxicillin, or a family member had a reaction and they assumed the same would happen to them.
True penicillin allergy, a confirmed immune response triggered by penicillin or its derivatives like amoxicillin and ampicillin can cause hives, swelling, trouble breathing, or low blood pressure. But if your reaction was just a stomach ache, diarrhea, or a mild skin rash that went away on its own, it’s unlikely to be a real allergy. That’s important because avoiding penicillin unnecessarily limits your treatment options. Doctors often reach for broader-spectrum antibiotics when penicillin is ruled out, which can lead to more side effects, higher costs, and even antibiotic resistance.
Cephalosporin cross-reactivity, the risk of reacting to other antibiotics like cephalexin or ceftriaxone if you’re allergic to penicillin has been overestimated for decades. Modern studies show the risk is less than 1% for most people, even those with a confirmed penicillin allergy. That means you might still safely take a cephalosporin if needed—especially if you’ve never had a severe reaction. Testing with an allergist can clear up confusion and open up better treatment paths.
People with a documented anaphylaxis, a sudden, life-threatening allergic reaction involving multiple body systems to penicillin should carry an epinephrine auto-injector and wear a medical alert bracelet. But for most others, a simple skin test or oral challenge can confirm whether the allergy still exists. These tests are safe, quick, and often covered by insurance. If you’ve been told you’re allergic to penicillin but can’t remember the details of your reaction, or if it happened more than 10 years ago, you might be eligible for testing.
You’ll find real stories and practical advice in the posts below—from how to recognize a true reaction versus a side effect, to what antibiotics you can safely use instead, and how to talk to your doctor about getting tested. Some people thought they were allergic for years, only to find out they could’ve taken penicillin safely all along. Others learned how to manage their allergy without over-restricting their care. Whether you’re dealing with a recent reaction or just want to understand your medical history better, these guides give you the facts you need to make smarter choices.
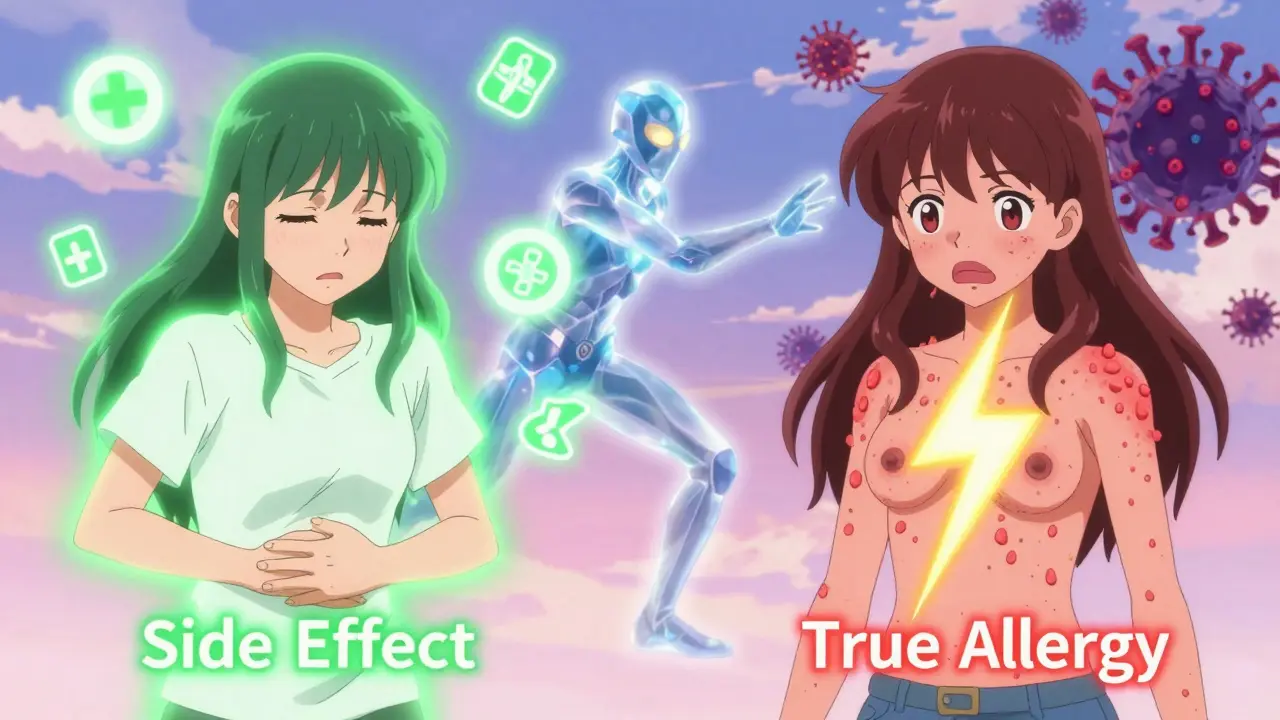
How to Tell a Side Effect from a True Drug Allergy
Learn how to tell the difference between a side effect and a true drug allergy. Most reactions aren't allergies-and mislabeling them can put your health at risk. Find out what symptoms really matter and how to get tested.
December 18 2025
Recognizing Signs of Drug Allergies and When to Seek Emergency Care
Learn how to spot true drug allergy symptoms vs. side effects, recognize life-threatening reactions like anaphylaxis, and understand when to get emergency help. Get the facts on diagnosis, testing, and why mislabeling is dangerous.
November 22 2025