Asthma Peak Flow Zone Calculator
Enter your personal best (PB) peak flow value and the current reading to determine your asthma severity zone and next steps.
Enter values to see your asthma severity zone and recommended actions.
Key Takeaways
- Stay calm, assess the situation, and act within minutes.
- Know how to use a rescue inhaler and when to give extra puffs.
- Follow the person’s asthma action plan before calling 911.
- Identify common triggers and keep emergency meds within reach.
- Practice the steps regularly so you’re ready for the real thing.
What Exactly Is an Asthma Attack?
Asthma attack is a sudden worsening of asthma symptoms caused by airway inflammation and muscle tightening. During an attack, the airways narrow, making it hard to breathe, and the person may experience wheezing, coughing, chest tightness, and rapid breathing.
Typical signs include:
- Shortness of breath that worsens quickly
- High‑pitched wheeze heard on exhalation
- Feeling of a “tight chest” or “belt around the chest”
- Persistent cough, especially at night
- Difficulty speaking full sentences
When you spot these symptoms, act fast. Delays of even a few minutes can turn a manageable flare‑up into a life‑threatening emergency.
Immediate Steps to Take
- Stay calm and reassure the person. Anxiety can tighten airways further.
- Ask if they have a rescue inhaler (usually a blue‑or‑yellow metered‑dose inhaler).
- If the inhaler is within reach, help them sit upright and take the first puff.
- Count to 10 seconds while they inhale slowly and hold their breath for about 3‑5 seconds.
- Wait 1‑2 minutes, then give a second puff if symptoms haven’t improved.
- If there’s no improvement after two puffs, give a third and a fourth puff at one‑minute intervals.
- Check the person’s breathing every minute. If it’s still getting worse, call emergency services (dial 911 in the U.S.) immediately.
- While waiting for help, keep the person calm, loosen tight clothing, and monitor their condition.
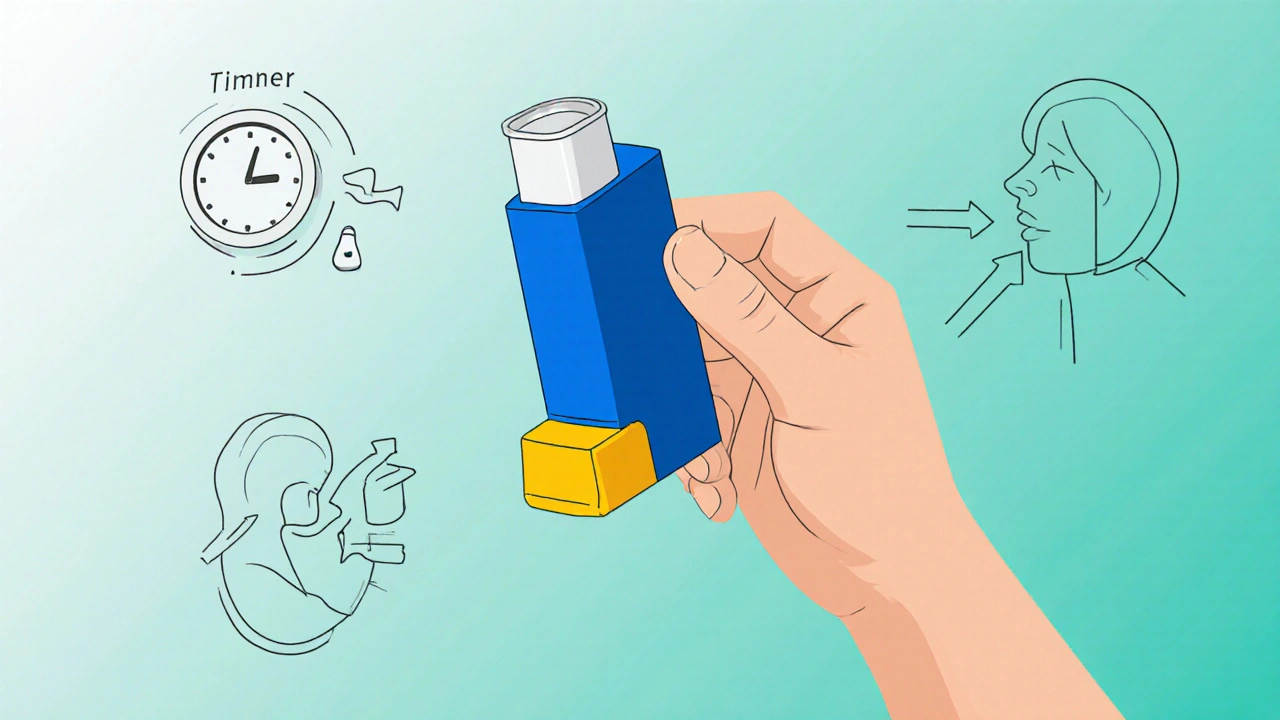
Using Rescue Medications Correctly
Most people carry a rescue inhaler that delivers a short‑acting bronchodilator, such as albuterol. Here’s how to get the most out of it:
- Shake the inhaler. This mixes the medication evenly.
- Attach a spacer if one is available; it helps more medicine reach the lungs.
- Press down once, and have the person breathe in slowly through the mouth.
- Hold the breath for a few seconds, then exhale slowly.
If the inhaler is empty, a bronchodilator tablet or nebulizer may be an option, but those are usually only at home and require a prescription.
When to Call Emergency Services
Even with quick inhaler use, some attacks need professional help. Call emergency services if:
- The person can’t speak more than a few words.
- Blue‑tinted lips or fingernails appear.
- There’s no improvement after two to four puffs.
- They’re using an epinephrine auto‑injector and still feel short‑of‑breath.
- They lose consciousness or have a seizure.
When you call, give the dispatcher the person’s name, age, exact location, and details about the medication used.
The Power of an Asthma Action Plan
Every asthma patient should have a written asthma action plan. It outlines:
- Daily controller medication doses.
- Peak flow zones (green, yellow, red) and what each means.
- Exact steps for mild, moderate, and severe symptoms.
- When to call a doctor versus emergency services.
Keep the plan on the fridge or in a medical bag. During an attack, pull it out and follow the instructions word‑for‑word. It removes guesswork and speeds up the response.

Additional Tools: Peak Flow Meter and Epinephrine Auto‑Injector
A peak flow meter measures how fast air leaves the lungs. Regular readings help spot worsening asthma before an attack.
- Take a reading at the same time each day.
- Compare the result to the personal best (PB) value.
- If the reading falls below 80% of PB (yellow zone), use a rescue inhaler and monitor closely.
- Below 50% (red zone) - treat as a severe attack and call emergency services.
Some people at high risk also carry an epinephrine auto‑injector. While it’s primarily for severe allergic reactions, it can momentarily widen airways during a life‑threatening asthma flare‑up. Use it only if the asthma action plan advises it and the inhaler isn’t helping.
| Feature | Rescue Inhaler (Albuterol) | Epinephrine Auto‑Injector |
|---|---|---|
| Primary Use | Relieve asthma bronchoconstriction | Treat severe allergic reaction / emergency asthma |
| Onset of Action | 1-3 minutes | 30 seconds-1 minute |
| Duration | 4-6 hours | 15-20 minutes |
| Typical Dose | 90‑150µg per puff (1‑2 puffs) | 0.15mg (auto‑injector) |
| Administration | Inhalation (mouth) | Intramuscular injection (thigh) |
| Side Effects | Tremor, rapid heartbeat | Palpitations, anxiety, sweating |
Preventing Future Attacks
Prevention is half the battle. Here are practical steps to lower the risk:
- Identify triggers. Common culprits are pollen, pet dander, smoke, cold air, strong odors, and viral infections.
- Use air purifiers and keep windows closed during high pollen days.
- Maintain a clean home-wash bedding weekly, vacuum with HEPA filters.
- Encourage the person to take controller medication exactly as prescribed.
- Schedule regular check‑ups; doctors can adjust doses based on peak flow trends.
- Teach the whole household how to use the inhaler and read the action plan.
When you know the “why” behind each attack, you can intervene before the breathing gets hard.
Frequently Asked Questions
What should I do if the person doesn’t have their inhaler?
Try to locate a backup inhaler (many families keep an extra at home or in the car). If none is available, use a nebulizer if you have one, or call emergency services immediately. Keep an epinephrine auto‑injector handy if the asthma action plan permits its use.
Can I give the person water during an attack?
Small sips are okay if the person can swallow safely, but large amounts of liquid can make the airway feel tighter. Focus on medication first; give water only after breathing improves.
How many puffs of a rescue inhaler are safe?
Most guidelines allow up to four puffs in a single episode, spaced one minute apart. If symptoms persist after four puffs, treat it as a severe attack and call 911.
What is the role of a peak flow meter during an emergency?
A peak flow reading in the red zone (<50% of personal best) confirms a severe attack and signals that emergency help is needed, even if the person feels slightly better after medication.
Should I lay the person flat?
Never lay them flat. Sitting upright opens the airways; if they feel faint, have them lean slightly forward while staying seated.
Helping someone through an asthma attack isn’t about being a medical professional; it’s about staying calm, acting fast, and following a clear plan. Keep the essential tools (inhaler, spacer, action plan) within reach, practice the steps regularly, and you’ll be ready the next time an attack strikes.


Fredric Chia
October 12, 2025 AT 23:27The guide accurately enumerates the steps, yet omits critical dosage thresholds.
Hope Reader
October 22, 2025 AT 00:47Wow, because we all keep a spare inhaler in the pantry, right? 😏
Emer Kirk
October 31, 2025 AT 01:07I can’t even begin to describe the panic that hits when you see someone struggling to breathe it’s like the world collapses
Roberta Saettone
November 9, 2025 AT 02:27First, verify that the person is indeed having an asthma exacerbation and not a simple shortness of breath from exertion.
If the inhaler is within reach, remove the cap and shake it vigorously for at least three seconds.
Encourage the patient to assume an upright seated position rather than a supine one, as gravity aids airway opening.
Administer the first puff and instruct a slow, deep inhalation followed by a three‑second breath hold.
Wait approximately ten seconds before delivering a second puff, assessing for any improvement in wheeze or speech.
Should symptoms persist, repeat the process up to a total of four puffs, spacing each one minute apart.
If after the fourth puff the individual remains in the red zone-unable to speak more than a few words, lips turning cyanotic-dial emergency services without hesitation.
Meanwhile, loosen any restrictive clothing and keep the environment calm; anxiety only worsens bronchoconstriction.
A spacer, when available, dramatically increases pulmonary deposition of the medication, so use it if you have one.
Document the peak flow reading before and after treatment; this data guides future action plans.
Remember that a rescue inhaler provides rapid bronchodilation but does not replace daily controller therapy.
If the inhaler is empty, a nebulized bronchodilator or an epinephrine auto‑injector, if prescribed, becomes the next line of defense.
Never underestimate the value of a well‑rehearsed asthma action plan; it eliminates guesswork during crises.
Educate all household members on these steps annually, because the best defense is preparedness.
And, of course, thank the person for remaining calm-cooperation can be the difference between a quick recovery and a hospital admission.
Sue Berrymore
November 18, 2025 AT 03:47Listen up, team! When someone’s airway is closing, you have to be the calm in the storm, the fire‑starter for confidence, and the relentless cheerleader who refuses to let panic win-so step up, follow the steps, and remember that every disciplined action today could be the lifesaver tomorrow.
Jeffrey Lee
November 27, 2025 AT 05:07Honestly, if the US had better public health education we wouldn’t need this on‑line guide-people would already know the exact dose of albuterol to take, the exact timing, and they’d be prideful enough to follow it without hesitaton. It’s not rocket science, it’s common sense, and it’s about time America got its act together.
Ian Parkin
December 6, 2025 AT 06:27While the instructions are thorough, I would recommend incorporating a brief reminder about the importance of regular controller medication, as this can dramatically reduce the frequency of acute episodes, even though occasional typographical errors may slip through unnoticed.
Julia Odom
December 15, 2025 AT 07:47Picture this: a bright sunrise, a gentle breeze, and a well‑prepared caregiver who knows every nuance of the inhaler’s choreography-this vivid scenario underscores how essential it is to transform routine practice into an artful performance for the loved one’s well‑being.
Danielle Knox
December 24, 2025 AT 09:07Oh sure, because everyone reads medical manuals before a crisis-let’s all just ignore the common sense that breathing is important, right?
Mark Evans
January 2, 2026 AT 10:27I completely understand how overwhelming it can feel, and I want to assure you that taking these steps calmly will make a huge difference for your loved one’s safety.
Alyssa Matarum
January 11, 2026 AT 11:47Grammar matters; the guide is clear.
Mary Akerstrom
January 20, 2026 AT 13:07Absolutely love how you keep it simple and to the point it really helps people stay focused
Delilah Allen
January 29, 2026 AT 14:27In the grand tapestry of human health, each breath is a thread; when that thread frays, we are reminded of our fragility, yet also of our resilience, for the act of assisting during an asthma attack becomes not merely a medical response, but a moral imperative, a testament to our collective responsibility, and an affirmation that we, as a society, can rise above the momentary panic to enact measured, compassionate care.
Nancy Lee Bush
February 7, 2026 AT 15:47The dedication you show, the calm you maintain, the precision of each inhaler puff-it all sings a hopeful melody of survival, and that optimism is contagious, lighting the room like a sunrise, brightening the path forward 😊
Dan Worona
February 16, 2026 AT 17:07One has to wonder why the pharmaceutical industry pushes inhalers as the sole solution while quietly suppressing alternative natural therapies that could empower patients beyond the emergency room cycle.
Chuck Bradshaw
February 25, 2026 AT 18:27Let me be clear: the physiology of bronchoconstriction is elementary, yet many still stumble because they ignore the simple fact that a properly timed puff can reverse the cascade within minutes.