Opioids During Pregnancy: Risks, Alternatives, and What You Need to Know
When you're pregnant and dealing with chronic pain, opioids during pregnancy, a class of powerful pain-relieving drugs that include oxycodone, hydrocodone, and methadone. Also known as narcotics, they can provide relief—but they also carry serious risks for your unborn child. The Centers for Disease Control and Prevention reports that nearly 1 in 5 pregnant women in the U.S. are prescribed opioids, often without fully understanding the long-term impact on the baby.
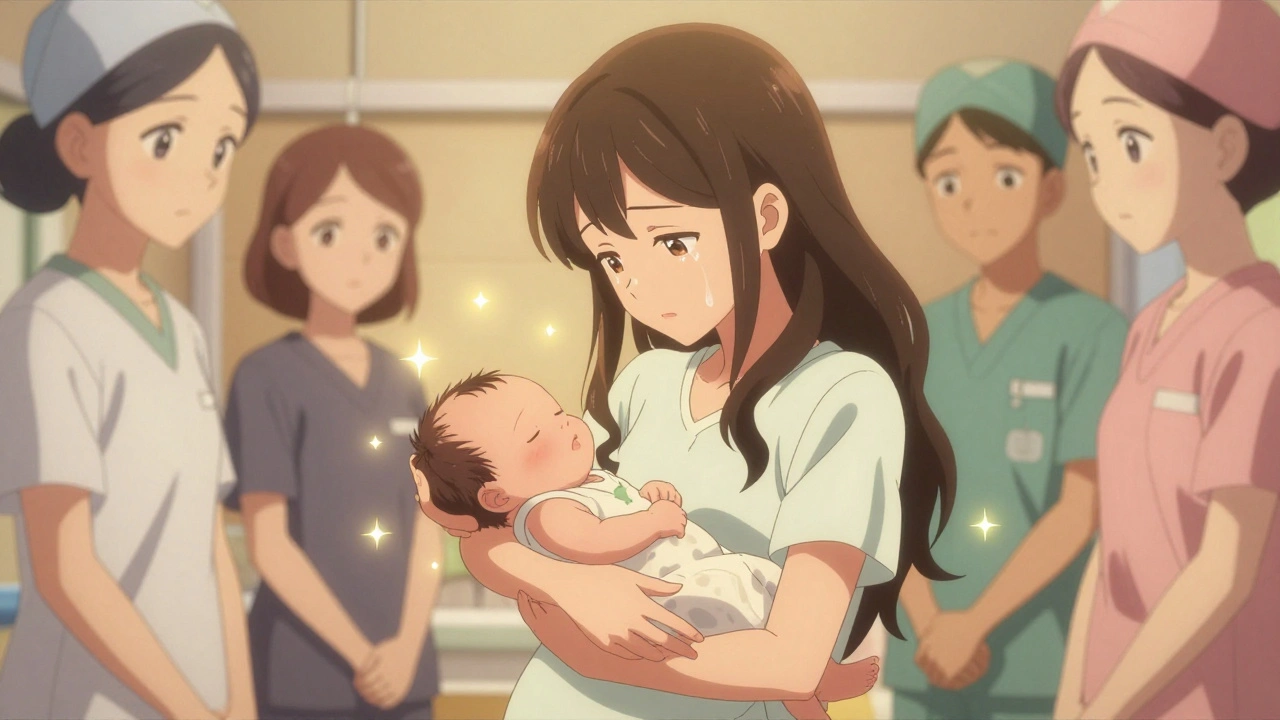
One of the biggest concerns is neonatal abstinence syndrome, a group of conditions that occur when a baby is exposed to opioids in the womb and goes through withdrawal after birth. Symptoms include excessive crying, tremors, feeding problems, and even seizures. These aren’t rare side effects—they happen in up to 60% of babies born to mothers using opioids regularly. And it’s not just about the dose; timing matters too. Using opioids in the third trimester increases the risk dramatically. Even prescribed opioids, taken exactly as directed, can cause this.
But here’s the thing: stopping opioids cold turkey can be just as dangerous. Sudden withdrawal can trigger preterm labor or miscarriage. That’s why pain management during pregnancy, a tailored approach that balances relief with safety is so critical. Some women are switched to methadone or buprenorphine—medications proven to stabilize both mother and baby better than street drugs or unmonitored prescriptions. These aren’t perfect, but they reduce the risk of overdose, improve prenatal care access, and lower the chance of complications.
Many women don’t realize they’re at risk until it’s too late. Opioids are often prescribed after a dental procedure, a car accident, or for back pain—situations where the long-term effects on pregnancy aren’t discussed. If you’re pregnant and taking any opioid, even a short-term prescription, talk to your provider. Ask if there’s a non-opioid option. Is acetaminophen enough? Could physical therapy help? Are there non-drug therapies like acupuncture or nerve blocks that are safe?
And if you’re already on opioids and worried? Don’t panic. Don’t hide it. The goal isn’t to shame you—it’s to protect your baby. Doctors can help you taper safely, monitor your baby’s development, and connect you with support services. Many clinics now specialize in prenatal opioid care, offering everything from counseling to parenting classes.
The bottom line: opioids during pregnancy aren’t automatically a disaster, but they’re not harmless either. The key is awareness, planning, and working with someone who understands both your pain and your pregnancy. The posts below cover real cases, medical guidelines, and alternatives that actually work—so you’re not left guessing what to do next.
Opioids During Pregnancy: Risks, Withdrawal, and What You Need to Know
Opioids during pregnancy require careful medical management. Learn the risks of withdrawal, how medication-assisted treatment helps, what to expect after birth, and why stigma shouldn't stand in the way of care.
December 1 2025