Atrial Flutter: Symptoms, Causes & Treatment Options
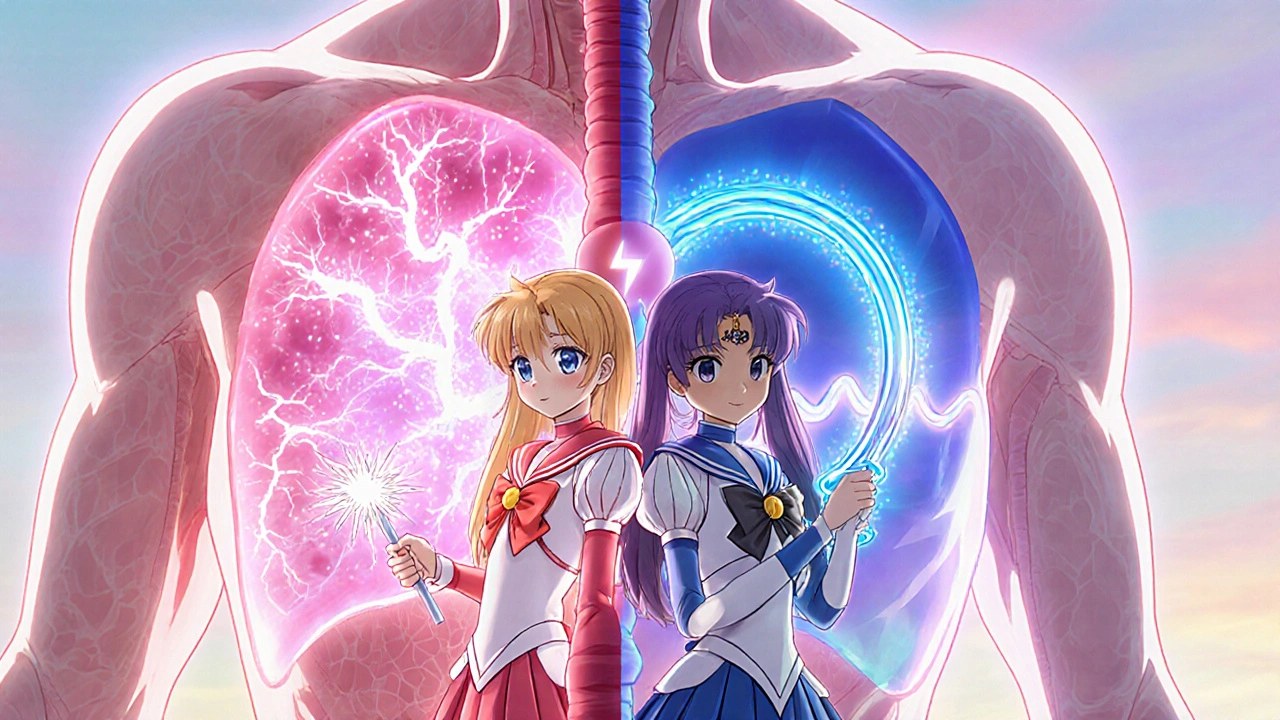
When dealing with Atrial Flutter, a fast, regular heart rhythm that originates from a circular electrical circuit in the atria. Also known as atrial tachycardia, it can cause palpitations, shortness of breath, and fatigue. This condition belongs to the broader group of cardiac arrhythmia, any disturbance in the heart’s normal rhythm, and is closely linked to atrial fibrillation, an irregular, often rapid heart rhythm that shares similar risk factors. Managing Atrial Flutter often requires anticoagulant therapy, medication that reduces blood clot risk because the fast atrial rate can promote clot formation. Additionally, an electrophysiology study, a minimally invasive test that maps the heart’s electrical pathways helps pinpoint the circuit and guides treatment decisions. In short, atrial flutter encompasses a specific rhythm disorder, requires careful assessment, and often leads to targeted interventions.
How Atrial Flutter Is Detected and Understood
Doctors usually spot atrial flutter during a routine ECG, where the hallmark “saw‑tooth” pattern appears between the P waves. If symptoms are vague, a Holter monitor can capture intermittent episodes over 24‑48 hours. The condition often co‑exists with atrial fibrillation; patients may swing between the two rhythms, making diagnosis tricky. An electrophysiology study not only confirms the flutter circuit but also distinguishes it from other supraventricular tachycardias. Risk factors mirror those of other cardiac arrhythmias: high blood pressure, coronary artery disease, and structural heart changes like enlarged atria. Lifestyle contributors such as excessive alcohol, sleep apnea, and chronic stress can tip the balance toward flutter. Understanding these triggers is key because addressing the underlying cause—like controlling hypertension—can lower recurrence rates. Moreover, identifying whether the flutter is typical (counter‑clockwise) or atypical guides the choice of ablation strategy, linking the diagnostic phase directly to therapeutic planning.
Treatment starts with rate‑control medications; beta‑blockers and calcium‑channel blockers slow the heart’s response to the rapid atrial signal, giving patients relief from palpitations. Because the flutter beats can cause blood to pool and clot, anticoagulant therapy is usually prescribed, especially for patients over 65 or with a history of stroke. For many, catheter ablation offers a curative option: using radiofrequency energy to interrupt the flutter circuit, the procedure restores normal rhythm in over 90 percent of cases. Post‑ablation, patients often continue on short‑term antiarrhythmic drugs to prevent early recurrence, then transition to routine follow‑up ECGs. Lifestyle tweaks—regular exercise, weight management, limiting caffeine—support long‑term success. The collection below dives deeper into each of these areas, offering practical advice on medication choices, monitoring strategies, and when to consider an ablation. Explore the articles to get clear, actionable guidance tailored to your situation.
Atrial Fibrillation vs Atrial Flutter: Key Differences, Symptoms & Treatment
Learn the key differences between atrial fibrillation and atrial flutter, their symptoms, risk factors, diagnosis, and treatment options in a clear, practical guide.
October 23 2025