Thiazide Diuretic Selector
Fill in patient details to get recommendation
Explanation will appear here based on selection
| Drug | Dosage | Half-life | Potassium Impact | CV Outcome Benefit |
|---|---|---|---|---|
| Hydrochlorothiazide | 12.5–50 mg | 6–15 hrs | Moderate loss | Modest |
| Chlorthalidone | 12.5–25 mg | 40–60 hrs | Higher loss | Strong |
| Indapamide | 1.5–2.5 mg | 14 hrs (action ~24) | Lowest loss | Strong |
| Metolazone | 2.5–5 mg | Long acting | Minimal | Strong |
Key Takeaways
- Hydrochlorothiazide (HCTZ) is effective for mild‑to‑moderate hypertension but may be less potent than newer thiazides.
- Chlorthalidone and indapamide generally provide longer blood‑pressure control and lower cardiovascular risk.
- Kidney function, electrolyte balance, and dosing convenience drive the choice of alternative.
- Loop diuretics such as furosemide are reserved for severe edema or renal impairment.
- Discuss side‑effects and drug interactions with a prescriber before switching.
What Is Hydrochlorothiazide?
When treating high blood pressure, Hydrochlorothiazide is a thiazide diuretic that helps the kidneys eliminate excess sodium and water. It was approved in the 1960s and quickly became a first‑line option because it’s cheap and works well for many patients.
HCTZ works by inhibiting the sodium‑chloride transporter in the distal convoluted tubule, leading to modest diuresis, reduced plasma volume, and lower peripheral resistance. The net effect is a drop in systolic and diastolic pressure, usually around 5-10mmHg.
Why Look at Alternatives?
Even though HCTZ is widely used, clinicians notice a few quirks. Its half‑life is short (6-15hours), so blood‑pressure control can wane toward the end of the day. Some patients develop low potassium or higher uric acid, which can trigger gout. And large‑scale studies suggest that newer thiazides may beat HCTZ at preventing heart attacks and strokes.
That’s why doctors often consider hydrochlorothiazide alternatives when a patient’s blood pressure stays high, side‑effects pile up, or kidney function changes.
Top Thiazide‑Like Alternatives
Chlorthalidone
Chlorthalidone is a long‑acting thiazide‑type diuretic with a half‑life of 40-60hours. Because it stays in the bloodstream longer, patients often need only once‑daily dosing, and blood‑pressure control remains steadier over 24hours.
Clinical trials (e.g., ALLHAT) showed chlorthalidone reduced the risk of heart failure more than HCTZ. It does, however, carry a higher risk of low potassium, so monitoring is key.
Indapamide
Indapamide combines thiazide activity with a mild vasodilating effect. Its half‑life is about 14hours, but its “half‑life of action” stretches longer because of its lipophilic nature.
Studies in elderly patients indicate indapamide lowers systolic pressure as well as HCTZ while causing fewer metabolic disturbances (potassium loss, glucose rise). It’s often the go‑to choice for patients with diabetes or metabolic syndrome.
Metolazone
Metolazone is a thiazide‑like diuretic that remains effective even when kidney function drops below a GFR of 30mL/min. That makes it useful in chronic kidney disease (CKD) where HCTZ loses potency.
Because it’s potent, clinicians start with low doses (2.5mg) and watch electrolytes closely.
When a Loop Diuretic Is the Better Fit
Furosemide is a loop diuretic that works high up in the nephron, producing a much stronger diuresis. It’s prescribed for acute pulmonary edema, severe heart failure, or when a thiazide can’t move enough fluid.
Loop diuretics are not first‑line for hypertension because their effect on blood pressure is less predictable, but they become essential when fluid overload dominates the clinical picture.
Side‑Effect Profile: How the Drugs Compare
| Attribute | Hydrochlorothiazide | Chlorthalidone | Indapamide |
|---|---|---|---|
| Typical daily dose | 12.5-50mg | 12.5-25mg | 1.5-2.5mg |
| Half‑life (hrs) | 6-15 | 40-60 | 14 (action up to 24) |
| Potassium‑sparing effect | Moderate loss | Higher loss | Lowest loss |
| Evidence for CV outcome benefit | Modest | Strong (ALLHAT) | Strong (HYVET) |
| Best for patients with | Mild hypertension, low cost need | Resistant hypertension, heart‑failure risk | Diabetes, metabolic syndrome, elderly |
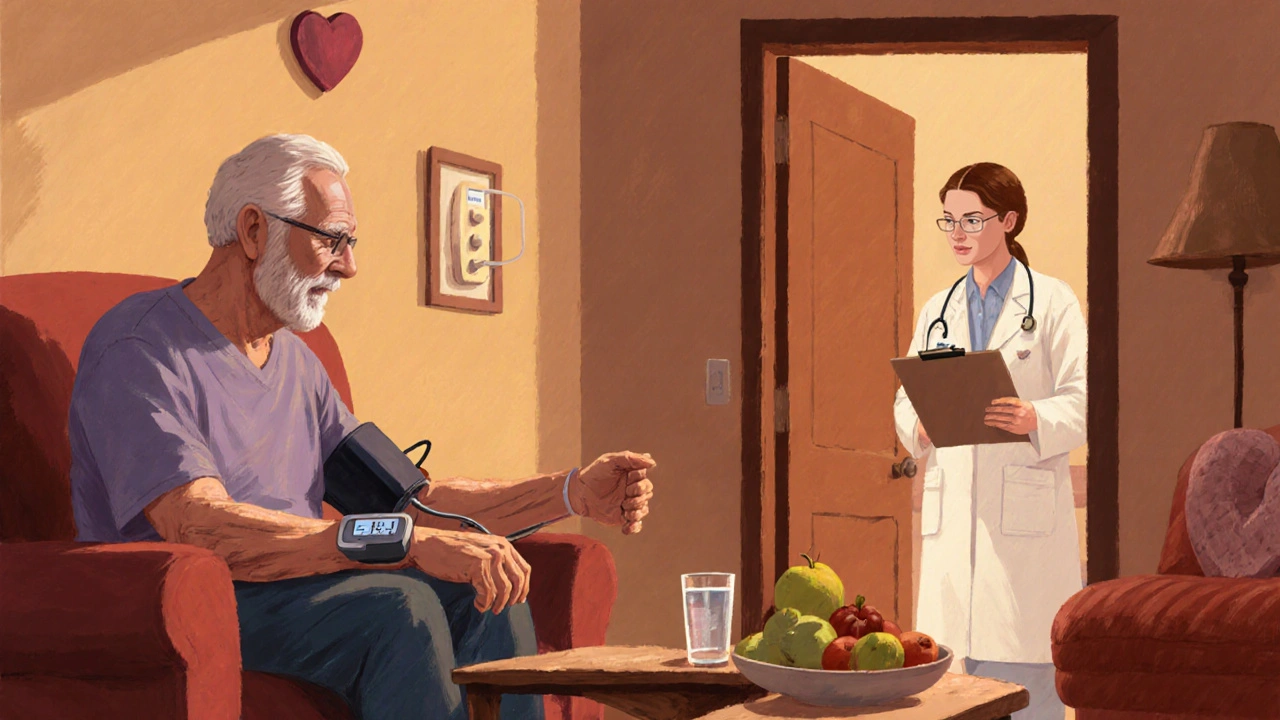
Practical Decision Guide
- Assess blood‑pressure control. If HCTZ drops pressure but the effect fades before bedtime, consider switching to chlorthalidone for its longer action.
- Check kidney function. When eGFR falls below 30mL/min, metolazone or a low‑dose thiazide‑like indapamide may retain efficacy, while HCTZ becomes ineffective.
- Watch electrolytes. If serum potassium repeatedly drops below 3.5mmol/L, indapamide’s gentler profile or adding a potassium‑sparing agent (e.g., spironolactone) can help.
- Consider comorbidities. Diabetes or gout patients benefit from indapamide’s smaller impact on glucose and uric acid.
- Factor in cost and access. HCTZ remains the cheapest option; insurance formularies often list it first. If out‑of‑pocket cost isn’t a barrier, newer agents may provide better long‑term outcomes.
Switching Safely
Never stop a diuretic abruptly without a plan. The typical switch protocol looks like this:
- Start the alternative at a low dose (e.g., chlorthalidone 12.5mg).
- Maintain the current HCTZ dose for 3‑5days to avoid a sudden fluid shift.
- Discontinue HCTZ and monitor blood pressure, weight, and electrolytes weekly for the first month.
- If dizziness or low blood pressure occurs, reduce the new drug’s dose by half and re‑evaluate.
Always involve your prescriber; some patients need a brief period of combination therapy before fully transitioning.
Frequently Asked Questions
Is Hydrochlorothiazide still a good first‑line choice?
Yes, for many people with mild‑to‑moderate hypertension HCTZ works well, is inexpensive, and has decades of safety data. It’s often the starting point before assessing whether a longer‑acting thiazide would give better control.
When should I consider Chlorthalidone over HCTZ?
If your blood pressure spikes in the afternoon or early evening, or if you have a history of heart‑failure, chlorthalidone’s longer half‑life provides steadier 24‑hour coverage and has stronger evidence for reducing cardiovascular events.
Can I use Indapamide if I have diabetes?
Indapamide is often preferred for diabetic patients because it has a minimal impact on blood‑sugar levels and causes the least potassium loss among thiazides. Regular glucose monitoring is still advised.
Why might a doctor add a loop diuretic?
When fluid overload (edema, pulmonary congestion) is severe, thiazides alone aren’t enough. Loop diuretics like furosemide move more water and sodium, quickly relieving symptoms. They’re also useful when kidney function is very low.
What are the common side‑effects to watch for?
Typical reactions include low potassium (hypokalemia), elevated uric acid (gout flare), increased blood sugar, and occasional dizziness from low blood pressure. Staying hydrated, eating potassium‑rich foods, and routine lab checks help catch problems early.
Bottom Line
Hydrochlorothiazide remains a solid, affordable option for many patients, but newer thiazide‑like agents often deliver steadier blood‑pressure control and better heart‑health outcomes. The right choice hinges on kidney function, electrolyte tolerance, comorbidities, and cost considerations. Talk with your healthcare provider about the pros and cons of each drug, and don’t hesitate to ask for a trial of an alternative if your current regimen isn’t hitting the mark.

Kitty Lorentz
October 6, 2025 AT 15:10I feel u could try a lower dose first
inas raman
October 11, 2025 AT 17:23Hey folks, just wanted to say that it’s cool to explore the different diuretics based on each person’s vibe. If your blood pressure is steady, HCTZ might be chill, but if you get those afternoon spikes, maybe a loop diuretic could help keep things even. Keep an eye on your kidneys and talk to your doc before swapping meds. Stay hydrated and stay positive!
Jenny Newell
October 16, 2025 AT 19:37The thiazide class, exemplified by hydrochlorothiazide, exhibits a prolonged half‑life and a modest natriuretic effect, making it suitable for patients with stable eGFR >60 mL/min. However, in cases of reduced renal clearance, the pharmacodynamic response may wane, prompting a switch to a loop diuretic or a potassium‑sparing agent.
Kevin Zac
October 21, 2025 AT 21:50I’ve seen many patients benefit from HCTZ when it’s paired with lifestyle changes. It’s easy to dose and inexpensive, which is a plus for compliance. That said, you gotta watch for electrolyte shifts, especially potassium loss, and adjust diet or add a supplement if needed.
Stephanie Pineda
October 26, 2025 AT 23:03Well Kevin, your point about cost‑effectiveness hits the nail on the head, yet we must also consider the philosophical balance between convenience and physiological nuance. A drug that’s cheap and simple can sometimes mask deeper renal dynamics, and the body’s response is a tapestry woven from genetics, diet, and stress levels. So while HCTZ shines in many cases, the art lies in tailoring therapy to the individual’s unique canvas.
Anne Snyder
November 1, 2025 AT 01:17When kidney function dips below 30 mL/min, I lean toward loop diuretics because they retain efficacy where thiazides falter. It’s also wise to monitor serum creatinine after any switch, just to keep the renal team in the loop.
Rebecca M
November 6, 2025 AT 03:30It is important, to be honest, to recognize that hydrochlorothiazide, while widely prescribed, does carry a risk of hypokalemia, hyperglycemia, and, in rare cases, severe allergic reactions; therefore, clinicians should conduct baseline laboratory assessments, counsel patients regarding potential side effects, and schedule regular follow‑up appointments to ensure safety and efficacy.
Bianca Fernández Rodríguez
November 11, 2025 AT 05:43Sure, Rebecca, but let’s not pretend the side‑effect profile is the only hurdle. Some patients develop tolerance faster than we anticipate, and the “one‑size‑fits‑all” narrative can be dangerous; we need to keep questioning the status quo.
Patrick Culliton
November 16, 2025 AT 07:57Honestly, I think people overcomplicate diuretic selection. If HCTZ works, stick with it – no need for endless switches unless there’s a clear clinical reason.
Andrea Smith
November 21, 2025 AT 10:10Dear community, kindly consider the importance of adhering to clinical guidelines when selecting a diuretic for hypertensive management; a structured approach ensures both safety and therapeutic effectiveness.
Gary O'Connor
November 26, 2025 AT 12:23i think the best way to pick is to see how your body reacts. some people get too low potassium with hctz, so they switch to a k‑sparing option.
Justin Stanus
December 1, 2025 AT 14:37From a purely clinical standpoint, the risk‑benefit analysis for HCTZ versus alternatives hinges on individual comorbidities, especially diabetes and gout, where thiazides may exacerbate underlying conditions.
Claire Mahony
December 6, 2025 AT 16:50While the data supports HCTZ for many, I’d caution against blanket recommendations; each patient’s profile demands a nuanced evaluation.
Andrea Jacobsen
December 11, 2025 AT 19:03In practice, I start with low‑dose HCTZ and titrate up if needed, monitoring electrolytes along the way; this balanced approach often yields good results without over‑complicating therapy.
Andrew Irwin
December 16, 2025 AT 21:17My experience shows that a gentle transition to a different class can be smoother for patients who are wary of side effects; patience is key.
Jen R
December 21, 2025 AT 23:30Honestly, the hype around newer diuretics is overrated – HCTZ does the job for most, as long as you keep an eye on potassium.
Joseph Kloss
December 27, 2025 AT 01:43One could argue that the philosophical underpinnings of diuretic choice reflect deeper societal trends toward quick fixes rather than holistic health.
Anna Cappelletti
January 1, 2026 AT 03:57Let’s stay optimistic – with proper monitoring, patients can safely navigate between HCTZ and its alternatives, achieving better blood pressure control while minimizing side effects.
Dylan Mitchell
January 6, 2026 AT 06:10Alright, gather round, because this is going to be a saga of diuretic drama you won’t forget.
First, let’s set the stage: hydrochlorothiazide struts onto the scene like the seasoned veteran, cheap, reliable, and always ready to lower that stubborn blood pressure.
But then enters the loop diuretic, sulking in the shadows, promising a stronger punch for those with compromised kidneys.
Our audience, the patients, are left wondering which hero to cheer for.
Enter the potassium‑sparing antagonist, the quiet one who refuses to let the electrolytes run wild.
Meanwhile, the witty sidekick, the thiazide‑like indapamide, whispers, “I’ve got a longer half‑life, just in case you need a steady ride.”
The plot thickens as comorbidities, like diabetes and gout, swoop in like plot twists, demanding a rewrite of the script.
Doctors, the directors, must balance cost, side effects, and patient preferences, like juggling flaming torches while riding a unicycle.
And don’t forget the ever‑present lab results, those relentless reporters that yell, “Potassium low!” or “Creatinine rising!” at the worst possible moments.
Yet, in the climax, a patient finds harmony by switching from HCTZ to a low‑dose loop, guided by diligent monitoring.
Or perhaps the hero stays put, adding a modest potassium supplement, and lives happily ever after.
Either way, the moral of the story is simple: there is no one‑size‑fits‑all, only personalized narratives.
So, choose your diuretic wisely, keep those labs in check, and remember that every medication choice writes its own chapter in your health saga.