Weight Loss Estimator for GLP-1 Medications
When you think of diabetes medications, you probably picture pills that lower blood sugar. But today, some of the most talked-about drugs in medicine aren’t just helping people with diabetes-they’re transforming how we treat obesity. Drugs like semaglutide and
How GLP-1 Agonists Actually Work
GLP-1 agonists mimic a natural hormone your body makes after eating. This hormone, called glucagon-like peptide-1, tells your pancreas to release insulin-only when blood sugar is high. That’s why these drugs rarely cause dangerous low blood sugar, unlike older diabetes meds. But that’s just the start. They also slow down how fast your stomach empties. Ever notice how full you feel longer after eating a meal? That’s this hormone at work. And here’s the real game-changer: they reach your brain and quiet down hunger signals. People on these drugs don’t just eat less-they stop craving junk food. It’s not willpower. It’s biology.
Think of it like this: your brain used to scream for more food every few hours. Now, it’s whispering, "I’m good." That’s why people report losing weight without feeling hungry. It’s not starvation. It’s regulation.
Weight Loss Numbers You Can’t Ignore
Let’s get specific. In clinical trials, people with obesity and type 2 diabetes who took tirzepatide a dual GLP-1/GIP agonist approved for weight loss under the brand name Zepbound lost an average of 11.6% of their body weight over 72 weeks. That’s like a 220-pound person dropping nearly 25 pounds. Even more striking? About 60% of participants on the highest dose lost 20% or more of their starting weight. That’s not modest. That’s life-changing.
For those without diabetes, the results are even more dramatic. In trials with only obese individuals (no diabetes), tirzepatide led to 20% weight loss on average. Semaglutide, sold as Wegovy a once-weekly GLP-1 agonist approved specifically for chronic weight management, helped people lose nearly 15% of their weight in the STEP-1 trial-more than six times what people lost with diet and exercise alone.
Compare that to older diabetes drugs. Sulfonylureas and insulin? They typically cause weight gain of 4 to 10 kilograms. GLP-1 agonists are the first class of diabetes meds that actually help you lose weight while controlling blood sugar. That’s why the American Diabetes Association now recommends them as first-line treatment for people with type 2 diabetes who also have obesity or heart disease.
Beyond the Scale: Heart, Brain, and Long-Term Survival
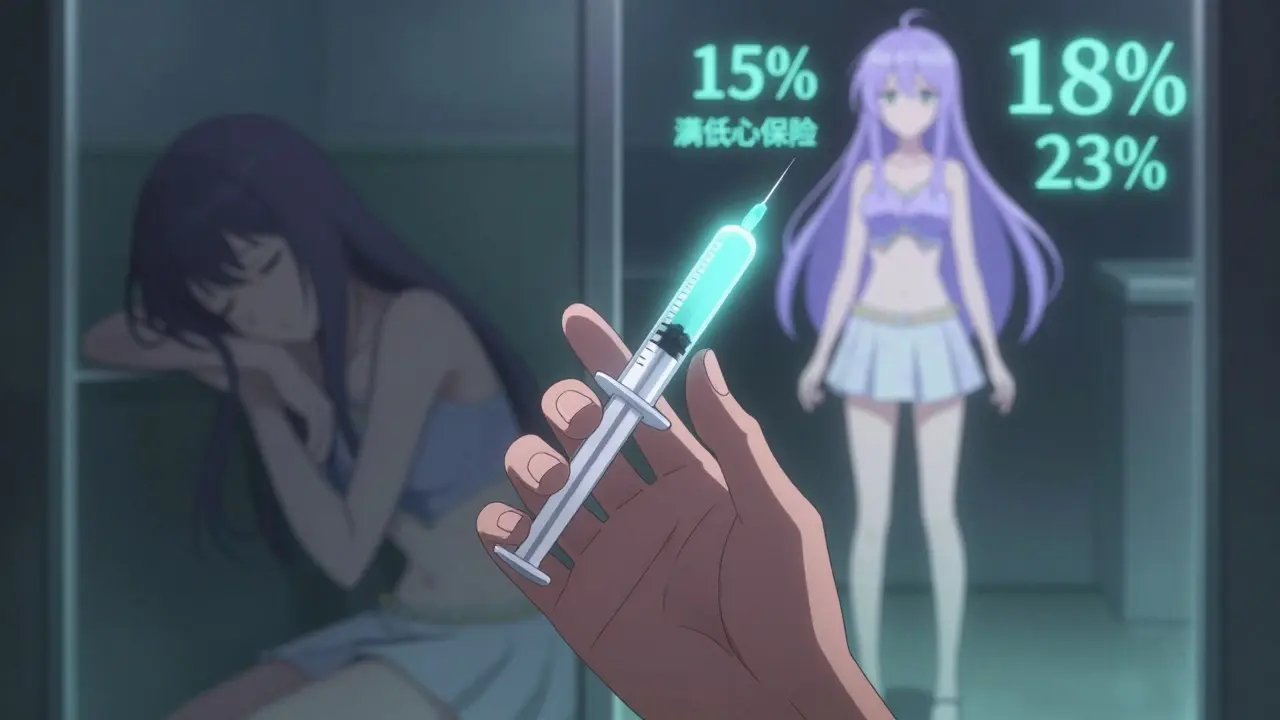
Weight loss is the headline. But the real story is what else these drugs are doing. A 2024 study from the University of Chicago analyzed over 15 GLP-1 agonists and found they didn’t just lower blood sugar-they cut the risk of major heart events like heart attacks and strokes by 12% to 18%. Mortality risk dropped by 8% to 14%. That’s not a side effect. That’s a therapeutic win.
And it’s not just the heart. A study of 2 million U.S. veterans found people on GLP-1 agonists had 23% fewer seizures, 17% lower risk of substance addiction (including alcohol and opioids), and 14% less suicidal thinking than those on other diabetes drugs. Researchers are now exploring whether these drugs could help with depression, addiction recovery, and even neurodegenerative diseases like Alzheimer’s.
They also improve blood pressure and cholesterol. LDL (the "bad" cholesterol) drops. Triglycerides fall. Blood pressure goes down. All without adding new medications. For someone with obesity, diabetes, and high blood pressure, this means fewer pills, fewer doctor visits, and a lower chance of complications down the road.
Who Benefits Most-and Who Doesn’t
These drugs aren’t magic bullets for everyone. They work best for people with:
- Type 2 diabetes and obesity
- Prediabetes with a BMI over 27
- Heart disease and excess weight
- Metabolic syndrome (high waistline, high blood pressure, high blood sugar)
For lean individuals without metabolic issues, the benefits don’t outweigh the risks. The weight loss is smaller, and side effects like nausea and vomiting are still common. That’s why doctors don’t prescribe them for people who are just "a little overweight." They’re meant for those with medical need.
And here’s the catch: if you stop taking them, you’ll likely regain most of the weight. Clinical data shows 50% to 70% of weight comes back within a year of quitting. That’s why these aren’t short-term fixes. They’re long-term tools-like blood pressure meds or statins. You don’t stop taking them because you feel better. You keep going because the risk returns.
The Side Effects Nobody Talks About Enough
Yes, these drugs work. But they’re not easy. Between 30% and 50% of users experience nausea, vomiting, or diarrhea-especially when starting. Most ease up after a few weeks, but for some, it’s enough to quit. Reddit threads are full of people saying, "I lost 30 pounds, but I couldn’t handle the constant nausea." Others report "Ozempic face"-a loss of facial fat that makes people look older or gaunt. Harvard Health found this happened in 42% of long-term users.
There’s also the risk of pancreatitis (about 0.5% to 1% of users) and gallbladder problems. These are rare, but real. And because these drugs slow digestion, they can interfere with how other medications are absorbed. That’s why you can’t just pick them up at the pharmacy without a doctor’s guidance.

Cost and Access: The Biggest Barrier
Wegovy costs around $1,349 a month without insurance. That’s more than $16,000 a year. Most people can’t pay that out of pocket. Insurance coverage is patchy. Some plans cover it only for diabetes, not weight loss. Others require you to try other meds first. In 2024, 58% of users reported insurance issues forcing them to ration doses or stop altogether.
Novo Nordisk’s Norditrac program helps eligible patients cover 75% of out-of-pocket costs. Telehealth services like Found and Calibrate bundle the drug with coaching and nutrition plans-but they cost $99 to $149 a month on top of the medication. For many, that’s still too much.
And supply shortages? Real. Manufacturers can’t keep up with demand. In 2023, global sales hit $35.7 billion. But only 2% of eligible people in the U.S. are even on these drugs. The gap between need and access is widening.
What’s Next? The Future of GLP-1 Drugs
Oral versions are coming. Right now, most GLP-1 drugs require a weekly injection. But Novo Nordisk is testing an oral semaglutide pill at 50 mg-five times stronger than the current version. If it works, it could change everything. No needles. No stigma. Just a daily pill.
Triple agonists are in the pipeline too. These drugs target GLP-1, GIP, and glucagon-all three hormones at once. Early data suggests they could double the weight loss of today’s best drugs. And researchers are testing them for non-alcoholic fatty liver disease (NASH), Parkinson’s, and even depression.
By 2030, analysts predict the GLP-1 market will hit $100 billion a year. That’s not hype. It’s demand. Obesity affects 42% of U.S. adults. And for the first time, we have a treatment that doesn’t just manage symptoms-it reverses the disease.
What You Need to Know Before Starting
- Start low, go slow. Most side effects fade if you begin with a tiny dose and increase gradually over 16 to 20 weeks.
- Combine with lifestyle changes. These drugs work better with good nutrition and movement. They’re not a replacement.
- Expect insurance battles. Know your plan’s rules. Ask about prior authorization and step therapy.
- Plan for the long term. If you stop, weight comes back. Think of this like a maintenance medication, not a cure.
- Watch for mental health changes. Some report improved mood. Others feel more anxious. Talk to your doctor.
These drugs are rewriting the rules of obesity treatment. They’re not perfect. They’re not cheap. But for millions, they’re the first real chance at lasting health. The question isn’t whether they work. It’s whether our healthcare system can make them accessible to the people who need them most.
Are GLP-1 agonists only for people with diabetes?
No. While they were first approved for type 2 diabetes, several GLP-1 agonists-like semaglutide (Wegovy) and tirzepatide (Zepbound)-are now FDA-approved specifically for chronic weight management in adults with obesity or overweight and at least one weight-related condition, even if they don’t have diabetes. The mechanism works the same: reducing appetite and slowing digestion. The difference is the dose and the indication on the prescription.
How long does it take to see weight loss results?
Most people start noticing reduced hunger and slight weight loss within the first 2 to 4 weeks. Significant weight loss (5% or more of body weight) typically happens between 12 and 20 weeks. Maximum results, like 10% to 20% weight loss, usually occur after 6 to 12 months of consistent use. The pace slows after the first few months, which is normal.
Can I take GLP-1 agonists if I have a history of thyroid cancer?
No. GLP-1 agonists carry a boxed warning for thyroid C-cell tumors in rodents. While it’s unclear if this risk applies to humans, these drugs are strictly avoided in people with a personal or family history of medullary thyroid cancer or in those with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Always disclose your full medical history to your doctor before starting.
Why do some people get "Ozempic face"?
"Ozempic face" refers to the loss of facial fat that can occur with rapid, significant weight loss. It’s not unique to GLP-1 agonists-it can happen with any drastic weight loss. But because these drugs cause consistent, prolonged weight loss, some users notice hollow cheeks, sagging skin, or deeper wrinkles. This is more common in older adults and those who lose 15% or more of their body weight. Dermatologists now offer fillers and skin-tightening treatments for those affected.
Do GLP-1 agonists affect mental health?
Yes-and in surprising ways. Studies show users report reduced cravings for sugar and alcohol, lower rates of substance use, and fewer thoughts of suicide. One 2024 study of veterans found a 14% drop in suicidal ideation among GLP-1 users. But some people experience anxiety, mood swings, or depression. The brain’s appetite centers are closely linked to emotional regulation. If you notice changes in your mood, talk to your provider. Don’t assume it’s "just weight loss."
What happens if I stop taking the drug?
Weight typically returns. Clinical trials show 50% to 70% of lost weight comes back within 12 months of stopping. This doesn’t mean the drug failed. It means obesity is a chronic condition, like hypertension or high cholesterol. For many, long-term use is needed to maintain results. Some doctors recommend tapering off slowly to minimize rebound weight gain.


Angie Datuin
February 8, 2026 AT 02:59Been on semaglutide for 8 months now. Not just the weight loss-though I dropped 42 lbs-but the way my cravings just... vanished. No more midnight ice cream raids. It’s like my brain finally got the memo that food isn’t a reward.
Ritteka Goyal
February 8, 2026 AT 10:56So this is just another american pharma scam right? We have natural ways in india like neem and turmeric and yoga and still you guys need some fancy injection? Also why is it so expensive? My cousin in mumbai can get a full month of ayurvedic treatment for 500 rupees lol
Chelsea Cook
February 10, 2026 AT 06:00Oh wow so now we’re treating obesity like it’s a disease you can inject away? Next they’ll be selling ‘willpower pills’ and ‘motivation patches.’
Ashlyn Ellison
February 11, 2026 AT 23:55I’ve seen people on this stuff and honestly? It’s not magic. Some people feel amazing. Others get nauseous 24/7. It’s not for everyone.
Joshua Smith
February 13, 2026 AT 02:22Just curious-has anyone tracked how long the weight stays off after stopping? I’m not against it, but I want to know if it’s sustainable or just a temporary fix.
John Watts
February 14, 2026 AT 15:15As someone who’s lived in 5 countries, I’ve never seen anything like this. In the US, obesity is treated like a moral failing. In Japan? It’s a public health metric. In Brazil? It’s part of the healthcare system. This drug is changing the game-but we need to stop treating it like a luxury.
Randy Harkins
February 15, 2026 AT 08:31Biggest win for me? My blood pressure dropped without even trying. I’m not even trying to lose weight anymore-I’m just living better. 🙌
Tatiana Barbosa
February 15, 2026 AT 19:59GLP-1 agonists are incretin mimetics that activate the GLP-1 receptor leading to enhanced insulin secretion and suppression of glucagon release. The central effect on appetite regulation via hypothalamic pathways is what makes them uniquely effective for obesity. But access? Still a nightmare. Insurance won’t cover it unless you have type 2 diabetes. Which is insane.
Ken Cooper
February 16, 2026 AT 10:45wait so this is like the new phentermine? i heard it works but like… what if you cant afford it? my friend tried it and said she had to sell her ps5 to pay for it. not cool. also i think its funny how everyone calls it ‘the weight loss drug’ like its a fad. its not. its medicine. just ask the diabetics.
Sam Dickison
February 17, 2026 AT 04:43Just a heads up: the GI side effects are real. I was fine for the first 2 weeks, then started vomiting every morning. My doc said it’s normal but… I’m not doing it again. Not worth it.
Brett Pouser
February 18, 2026 AT 23:41My abuela in Mexico City used to say, ‘The best medicine is a full plate and a full heart.’ I get the science. But I also miss when we treated health like community, not a product.
Camille Hall
February 19, 2026 AT 22:54For anyone worried about access or cost: I work with a nonprofit that helps people get these meds through patient assistance programs. DM me if you’re struggling. You’re not alone.