Imagine taking five pills a day just to manage your blood pressure, diabetes, and cholesterol. Now imagine taking just one. That’s the whole point of fixed-dose combination drugs-they bundle two or more medicines into a single tablet or capsule, so you don’t have to juggle multiple pills. But they’re not just about convenience. In many cases, they actually make treatment safer, more effective, and easier to stick with.
What exactly are fixed-dose combination drugs?
A fixed-dose combination drug, or FDC, is a single medicine that contains two or more active ingredients in set amounts. Think of it like a pre-mixed smoothie-you can’t change how much banana or spinach goes in. Once it’s made, the doses are locked in. You can’t take half a pill to reduce one drug without affecting the other.
This isn’t the same as taking two separate pills at the same time. FDCs are chemically and physically combined into one unit. Common examples include pills that mix a blood pressure drug like lisinopril with a diuretic like hydrochlorothiazide, or a diabetes medicine like metformin with sitagliptin. Even some HIV treatments are FDCs, combining three or four antivirals into one daily tablet.
The World Health Organization has been backing these since 2005, listing 18 FDCs on its Essential Medicines List. Today, that number keeps growing. The key rule? The combination must offer a real benefit-not just because it’s easier to make, but because it actually improves how patients do.
Why do these combinations even exist?
There are three big reasons FDCs were created: better results, fewer pills, and simpler routines.
First, some drugs work better together. Take tuberculosis treatment. Rifampicin and isoniazid are both powerful against TB, but when used alone, the bacteria can quickly become resistant. Together, they stop resistance from forming. That’s synergy. The same is true for antibiotics like amoxicillin and clavulanate-the second drug blocks the enzyme that makes the first one useless.
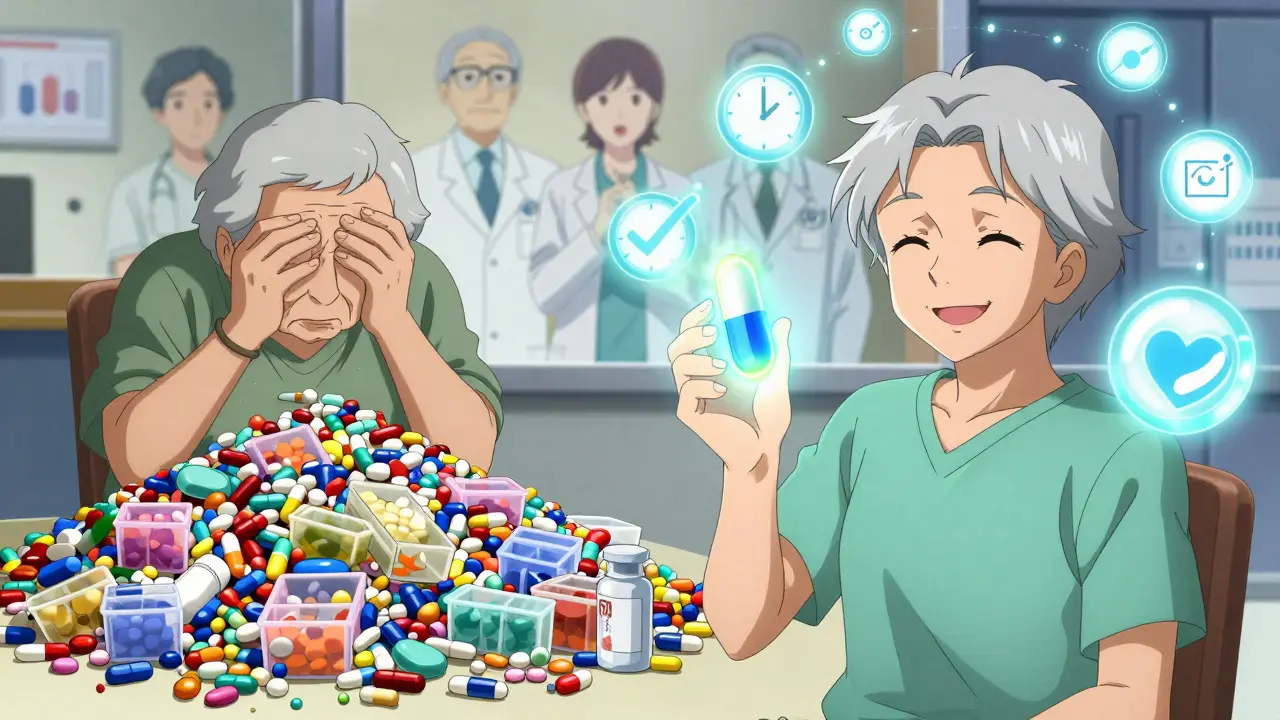
Second, fewer pills mean fewer chances to forget. Studies show people who take multiple pills daily are far more likely to skip doses. One study found that switching from three separate pills to one FDC improved adherence by nearly 30%. That’s huge for chronic conditions like heart disease or diabetes, where missing doses can lead to hospital stays or worse.
Third, it’s cheaper and less hassle. Fewer prescriptions mean fewer trips to the pharmacy, lower co-pays, and less time spent sorting pill organizers. For older adults or those on tight budgets, that’s not a small thing.
Are all FDCs created equal?
No. And that’s where things get messy.
Some FDCs are brilliant. Levodopa and carbidopa for Parkinson’s? Perfect. Carbidopa stops levodopa from breaking down too early, so more of it reaches the brain. That’s science-backed, life-changing.
But others? They exist because a drug company’s patent is about to expire. Instead of letting generics take over, they slap an old drug together with a new one, file for a new patent, and keep selling at high prices. Payers and doctors call these “lifecycle extension” strategies. They’re legal, but they don’t always help patients.
The FDA and European Medicines Agency require proof that each ingredient in an FDC actually contributes to the benefit. That means companies can’t just bundle drugs and call it a day. They need data-real clinical trials showing the combo works better than the individual drugs alone. Still, not all regulators are equally strict. Some FDCs on the market, especially in lower-income countries, lack solid evidence.
What are the downsides?
Fixed doses mean no flexibility. If your blood pressure drops too low on one component but you still need the full dose of the other, you’re stuck. You can’t adjust one without affecting the other. That’s a problem if your condition changes over time.
Also, side effects can pile up. One drug might cause dizziness, another might cause nausea. Together, you get both. And if the drugs have different ways they’re absorbed or cleared from the body, the combo might not work as smoothly as hoped.
Then there’s cost. Sometimes FDCs are more expensive than buying the two drugs separately-especially if one or both are available as cheap generics. A 2020 IQVIA report found that in some cases, patients paid 40% more for the combo than if they’d bought the pills on their own.
Where are FDCs most commonly used?
Cardiovascular disease leads the pack. About 40% of all branded FDCs are for high blood pressure, cholesterol, or heart failure. That’s because these conditions often require multiple drugs, and patients are older-more likely to forget pills.
Dermatology is another big area. Acne treatments often combine antibiotics with retinoids in one gel. Psoriasis creams mix steroids with vitamin D analogs.
HIV treatment was one of the first big wins for FDCs. In the early 2000s, patients had to take 10-20 pills a day. Now, many take just one. That single pill changed survival rates and quality of life.
Emerging areas? Cancer and neurodegenerative diseases. Researchers are testing FDCs that target multiple cancer pathways at once, or combine drugs to slow Alzheimer’s progression. But these are still early days.

How are they approved?
In the U.S., most FDCs use the FDA’s 505(b)(2) pathway. That means the company doesn’t have to start from scratch. If one or both ingredients are already approved, they can use existing safety data. But they still need to prove the combo works as intended.
That means new clinical trials-usually Phase 2 and 3-to show the fixed ratio is safe and effective. Between 2010 and 2015, over half of approved FDCs still needed full trials, even though they used older ingredients. The FDA isn’t cutting corners.
The WHO has its own checklist for what makes a good FDC:
- The drugs must work in different ways
- They must have similar how-long-they-last-in-the-body profiles
- The combo shouldn’t cause worse side effects than the drugs alone
- The doses must match what’s needed for the target group
If a combo doesn’t meet these, it shouldn’t be on the market. But in practice, some slip through.
What’s the future look like?
FDCs aren’t going away. In fact, they’re getting smarter.
Companies are now designing FDCs with better release profiles-slow-release versions that keep drug levels steady all day. Some are even testing FDCs with sensors that track if you took the pill, sending alerts to your doctor if you didn’t.
Payers are getting pickier. Insurance companies now demand proof that an FDC improves outcomes-not just convenience. They’re starting to reject FDCs that don’t show better hospitalization rates, fewer ER visits, or improved quality of life scores.
And global health agencies are pushing for more rational FDCs in low-income countries, especially for infections like TB and malaria. One FDC that kills two birds with one stone? That’s a win for public health.
But the bottom line hasn’t changed: if a combination doesn’t help patients more than the separate drugs, it shouldn’t exist. The goal isn’t to make pills easier to swallow-it’s to make lives easier to live.
Are fixed-dose combination drugs safe?
Yes, when they’re properly developed and approved. Regulatory agencies like the FDA and WHO require strong evidence that the combination is safer or more effective than taking the drugs separately. But not all FDCs meet that bar. Some are marketed more for business reasons than patient benefit. Always ask your doctor if the combo makes sense for your specific condition.
Can I adjust the dose of one drug in an FDC?
No. Because the doses are fixed, you can’t increase or decrease one component without changing the whole pill. If your doctor needs to tweak one drug-say, lower your blood pressure medicine but keep your cholesterol drug the same-you’ll need to switch to separate pills or find a different FDC.
Are FDCs cheaper than buying separate pills?
Sometimes, but not always. If both drugs in the combo are generic, buying them separately is often cheaper. FDCs can cost more because they’re branded, patented, or marketed as premium products. Always compare prices at your pharmacy. Some insurers even require you to try the generic versions first before covering the combo.
Why are FDCs common in HIV and TB treatment?
Because adherence is life-or-death. HIV and TB require long-term, multi-drug regimens. Missing doses can lead to drug-resistant strains that are harder and more expensive to treat. FDCs cut pill burden from 10+ pills down to one or two per day, making it far easier for patients to stick with treatment. Studies show this directly improves survival rates.
Do FDCs cause more side effects?
They can. Since you’re taking two drugs at once, you’re exposed to the side effects of both. For example, one drug might cause dizziness, another might cause stomach upset. Together, you get both. That’s why regulators require proof the combo doesn’t increase risk compared to separate use. But for many patients, the benefit of better control outweighs the side effects.
What should you do if you’re prescribed an FDC?
Ask three questions:
- Why this combo? What’s the evidence it works better than separate drugs?
- Can I take the ingredients separately if I need to adjust a dose later?
- Is there a cheaper generic option?
Don’t assume the FDC is automatically better. It might be. But it might also be a marketing move. Work with your doctor to make sure it’s the right fit for your body, your lifestyle, and your budget.



Priya Patel
January 10, 2026 AT 11:55One pill instead of five? Sign me up. My grandma takes so many pills she needs a spreadsheet and a GPS tracker. This is life-changing for people like her.
Sean Feng
January 11, 2026 AT 21:46Yeah but what if you need to adjust one drug? You’re stuck. That’s not convenience, that’s a trap.
Priscilla Kraft
January 12, 2026 AT 10:44Love this breakdown! 💯 Especially how they mentioned TB and HIV-FDCs literally saved lives in resource-limited settings. The WHO checklist is spot on. If a combo doesn’t meet those criteria, it shouldn’t be on the market. Simple.
Alfred Schmidt
January 13, 2026 AT 18:24Of course the pharma companies love this-they’re just extending patents under the guise of ‘patient convenience.’ They don’t care about your health, they care about your co-pay. This is capitalism in action.
Vincent Clarizio
January 14, 2026 AT 01:02Think about it-human beings are lazy by design. We forget keys, phones, birthdays. Why would we suddenly remember five different pills at five different times? Evolution didn’t prepare us for this. The body wants simplicity. The brain wants routine. The pill bottle? It’s just a relic of a time when we didn’t know better. FDCs aren’t just medicine-they’re a psychological hack. We’re not just treating disease anymore, we’re optimizing compliance. And if that means bundling drugs into a single capsule that feels like a victory, then maybe that’s the real breakthrough. Not the chemistry. Not the dosage. The fact that someone can swallow one thing and feel like they’ve won the day.
Sam Davies
January 14, 2026 AT 21:52Oh wow, a magic bullet that also magically costs 40% more? How quaint. Next they’ll sell us a ‘convenience’ toothpaste that combines floss, brush, and existential dread.
Christian Basel
January 16, 2026 AT 08:14Adherence metrics are the only KPI that matters here. The NNT for FDCs in hypertension is significantly improved-RR 0.78, CI 0.72–0.84-when compared to free combination regimens. The cost differential is negligible in high-income systems with tiered formularies. The real issue is regulatory arbitrage in LMICs where pharmacovigilance is under-resourced.
Alex Smith
January 17, 2026 AT 23:52Interesting. So if I’m on a combo pill and my BP drops too low, I can’t just reduce the diuretic? I have to go back to three pills? That’s… kind of a design flaw, isn’t it? Who decided this was a good trade-off?
Roshan Joy
January 19, 2026 AT 19:04My uncle in Delhi takes his TB meds as one pill now. He used to miss days. Now he takes it with his chai every morning. One pill. One habit. That’s all it took. This isn’t fancy science-it’s dignity.
Michael Patterson
January 19, 2026 AT 23:25Okay but what if you have kidney issues? Some of these combos arent tested on people with CKD. And now you're stuck with a pill you can't adjust? This is why people end up in the ER. Pharma doesn't care about real patients, only their profit margins. And doctors? They're just following the script.
Matthew Miller
January 21, 2026 AT 09:56Let’s be real: 80% of FDCs are patent evergreening scams. The other 20% are lifesavers. The problem isn’t the concept-it’s the lack of oversight. Who’s auditing these? Who’s tracking long-term outcomes? No one. Because money talks and science walks.
Jennifer Littler
January 23, 2026 AT 08:42As someone who works in hospital pharmacy, I see this daily. FDCs reduce medication errors, streamline discharge planning, and cut down on pill burden for elderly patients. But we have to be vigilant-some combos are just bad science wrapped in pretty packaging. Always check the evidence.
Jason Shriner
January 23, 2026 AT 14:37So we’ve turned medicine into a vending machine. You put in your symptoms, you get one pill. No thinking. No adjustments. No humanity. Just a little white capsule that says ‘you’re doing fine.’ But what if you’re not? What if you need to change? What if you’re just… human?
Adewumi Gbotemi
January 25, 2026 AT 12:33Here in Nigeria, we don’t have the luxury of choice. If a FDC works and is cheap, we use it. We don’t care if it’s branded or generic. We care if it keeps our mothers alive. That’s the real test.