When you’re sick and your doctor prescribes an antibiotic, you want it to work. Not half-work. Not barely work. Work. But if you’re drinking milk, eating yogurt, or grabbing a cheese stick with your pill, you might be sabotaging it - without even realizing it.
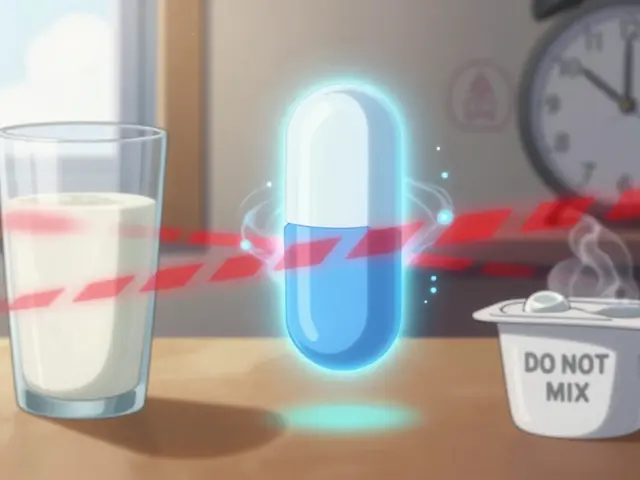
This isn’t a myth. It’s chemistry. And it’s been known for over 50 years. The calcium in dairy products binds tightly to certain antibiotics, forming a hard, insoluble lump in your gut. That lump doesn’t get absorbed. It just passes through. And if your antibiotic doesn’t get into your bloodstream, your infection doesn’t get treated. That’s not just inconvenient - it’s dangerous.
Which Antibiotics Are Affected?
Not all antibiotics react the same way with dairy. The big offenders are two classes: tetracyclines and fluoroquinolones.
Tetracyclines include older drugs like tetracycline and minocycline, and the more commonly used doxycycline. These were the first to be studied back in the 1960s. Calcium in milk, cheese, or yogurt latches onto tetracycline molecules like a magnet. Studies show this can slash absorption by 50% to 90%. Even doxycycline, which is less affected than its older cousins, still loses up to 30% of its effectiveness if taken with dairy.
Fluoroquinolones like ciprofloxacin (Cipro), levofloxacin (Levaquin), and moxifloxacin (Avelox) are just as vulnerable. One study found that milk reduced ciprofloxacin’s peak blood levels by 70%. Yogurt? That dropped it by 92%. That’s not a small drop - that’s nearly wiping out the drug’s power.
Other drugs like bisphosphonates (used for osteoporosis) behave the same way. But penicillins, amoxicillin, azithromycin, and most other antibiotics? They’re fine with dairy. No problem. So if you’re on one of those, go ahead and enjoy your yogurt. But if you’re on tetracycline or ciprofloxacin - hold off.
Why Does This Happen?
It’s all about the calcium. Dairy isn’t just milk. It’s cheese, cottage cheese, ice cream, kefir, and even some calcium-fortified plant milks like almond or soy. All of them contain high levels of calcium, magnesium, aluminum, or iron - what scientists call polyvalent cations.
These minerals have a strong chemical attraction to certain antibiotics. When they meet in your stomach or intestines, they form a complex - basically a tiny rock. Your gut can’t absorb rocks. So the antibiotic just sits there, useless, until it’s pooped out.
It doesn’t matter if you eat the dairy before or after the pill. If they’re in your system at the same time, they’ll bind. The timing isn’t about digestion speed - it’s about avoiding overlap in the gut. Even if you take your antibiotic with breakfast and have yogurt for a snack two hours later, you’re still risking the interaction.
How Long Should You Wait?
Timing isn’t vague. It’s specific. And it varies by drug.
For tetracyclines (including doxycycline): Take the pill at least 1 hour before eating dairy - or wait 2 hours after. Some experts recommend 3 hours for maximum safety, especially if you’re treating a serious infection like Lyme disease or a stubborn sinus infection.
For fluoroquinolones (like ciprofloxacin): Be stricter. Take the antibiotic 2 hours before dairy - and wait 4 to 6 hours after. That’s because fluoroquinolones are more sensitive to calcium than tetracyclines. A 2-hour gap isn’t enough. You need a full half-day buffer.
Here’s a simple trick: If you take your antibiotic in the morning, take it on an empty stomach - right when you wake up, before coffee or toast. Then wait until after lunch to have yogurt or cheese. If you take it at night, take it right before bed, and don’t have a bedtime snack with dairy. That’s the easiest way to avoid conflict.
And don’t forget: calcium-fortified orange juice, almond milk, or even some breakfast cereals can trigger the same reaction. Read labels. If it says “calcium added,” treat it like dairy.

What Happens If You Ignore This?
You might think, “I had a glass of milk with my pill once - what’s the big deal?” But this isn’t a one-time thing. It’s cumulative.
When your antibiotic levels stay low, the bacteria don’t die. They survive. And the ones that survive? They’re the toughest. They learn how to resist the drug. That’s how antibiotic resistance starts - not just from overuse, but from under-dosing.
Real-world cases prove this. Nurses on Reddit have shared stories of patients with Lyme disease who kept getting worse - until someone realized they were drinking milk with every dose of doxycycline. A 2023 study found that 22% of urinary tract infection treatment failures were linked to dairy timing mistakes. And a survey by the American Society of Health-System Pharmacists showed that 43% of patients never got clear instructions from their doctor about this.
It’s not just about the pill not working. It’s about turning a simple infection into a chronic problem. Or worse - creating a superbug that could spread to others.
What Do Experts Say?
Doctors, pharmacists, and health agencies all agree: timing matters.
The FDA, European Medicines Agency, and the Infectious Diseases Society of America all updated their guidelines in 2023 to stress specific time windows - not just “avoid dairy.” They want patients to know exactly when to separate the two.
Dr. Sarah Thompson, an infectious disease specialist at Johns Hopkins, says she’s seen multiple patients with recurring UTIs - all because they took ciprofloxacin with their calcium-fortified cereal. “It’s not their fault,” she says. “No one told them.”
Pharmacists are now using digital tools to help. Apps like Medisafe and MyMeds pop up alerts when you enter ciprofloxacin or doxycycline: “Wait 2 hours before or after dairy.”
Even pharmaceutical companies are responding. Extended-release versions of ciprofloxacin (Cipro XR) were developed to reduce this interaction - but they cost over $200 a prescription. The generic version? Around $16. So most people stick with the cheaper option - and need to be extra careful with timing.

Real-Life Solutions
Life doesn’t stop just because you’re on antibiotics. You still eat meals. You still like your yogurt. So how do you make it work?
Here’s what works for real people:
- Take tetracyclines in the morning on an empty stomach. Wait 2 hours before breakfast. Have your coffee, toast, and yogurt after lunch.
- If you take it twice a day, take the first dose in the morning before food, the second at bedtime - and skip dairy snacks after dinner.
- Use a timer. Set your phone to remind you: “Take pill now. No dairy for 2 hours.”
- Ask your pharmacist. They see this every day. They’ll tell you exactly what to avoid and when.
- Check your supplements. Calcium pills, multivitamins with iron or zinc - same problem. Take them at least 2 hours apart from your antibiotic.
One patient on Drugs.com wrote: “My UTI kept coming back until my pharmacist said, ‘Wait 4 hours after your cipro before yogurt.’ I did it. The infection cleared in two days.”
The Bigger Picture
This isn’t just about you. It’s about public health.
The World Health Organization calls antibiotic resistance one of the top global health threats. And timing mistakes with dairy? They’re a quiet contributor. Every time an antibiotic doesn’t work because of a missed gap, we’re helping resistant bacteria survive.
But here’s the good news: this is one of the easiest problems to fix. No new drug. No expensive test. Just a little planning. A 2-hour wait. A simple change in routine.
By 2025, digital tools and better labeling are expected to cut non-compliance in half. But until then - it’s on you to know the rules. And now you do.
Can I have yogurt with doxycycline if I wait a few hours?
Yes - but you need to wait at least 2 hours after taking doxycycline before eating yogurt. Even though doxycycline is less affected by calcium than older tetracyclines, dairy can still reduce its absorption by up to 30%. Waiting 2 hours ensures enough time for the antibiotic to be absorbed before calcium enters your system.
What if I accidentally took my antibiotic with milk?
If it was just once, don’t panic. Skip your next dairy meal and continue taking your antibiotic as prescribed. Don’t double up on your dose - that won’t help and could cause side effects. If you’re treating a serious infection and you’re unsure, contact your doctor or pharmacist. They may want to check your progress or extend your treatment.
Are plant-based milks like almond or oat milk safe?
Not necessarily. Many plant-based milks are fortified with calcium - sometimes even more than dairy milk. Always check the label for “calcium carbonate” or “tricalcium phosphate.” If it’s added, treat it like dairy. Stick to unfortified versions or wait the full 2-6 hours after your antibiotic.
Does cooking dairy change anything?
No. Heating milk or cheese doesn’t break down the calcium. Whether it’s melted on pizza, baked into a casserole, or stirred into soup - the calcium is still there. The interaction happens chemically, not physically. So cooked dairy still interferes with antibiotic absorption.
Can I take my antibiotic with water instead of milk?
Yes - and you should. Always take tetracyclines and fluoroquinolones with a full glass of plain water. Avoid tea, coffee, juice, or milk. Water doesn’t interfere. And it helps the pill move through your system without getting stuck. Some antibiotics can irritate your esophagus if they sit too long - water helps prevent that too.

Angel Molano
January 15, 2026 AT 05:05Stop eating cheese with your antibiotics. Seriously. It’s not that hard.
Gregory Parschauer
January 15, 2026 AT 17:43Oh wow, another ‘you’re killing the planet by drinking milk with your doxycycline’ lecture. Let me guess-you also wash your hands for 20 seconds while humming the alphabet and only use organic kale to wipe your butt? This isn’t medicine, it’s performative health cultism. I’ve taken cipro with yogurt for years and my UTIs vanished. Your ‘studies’ are funded by Big Pharma to sell you $200 XR versions. Wake up.
Also, calcium doesn’t ‘bind’ like magic glue-it’s a kinetic equilibrium. If you’re not vomiting or having diarrhea, your body absorbed enough. Your fear is peddled by pharmacists who get paid per consultation.
And don’t even get me started on ‘calcium-fortified almond milk.’ That’s just corporate greenwashing. Almond milk has 1% almonds. The rest is water, sugar, and guilt.
I’ve seen more people ruin their gut biome with probiotic yogurt than ever get antibiotic failure from dairy. You’re turning a minor pharmacokinetic quirk into a moral failing. Pathetic.
Vinaypriy Wane
January 16, 2026 AT 12:04I appreciate this post... truly. I’ve been on doxycycline for Lyme, and I didn’t know about the calcium thing until my pharmacist pulled me aside last week. I was having Greek yogurt every morning with my pill. I thought I was being healthy. Turns out, I was sabotaging my own recovery.
Now I take it at 7 a.m. on an empty stomach, and wait until after lunch. I’ve already noticed a difference-less fatigue, clearer head. Thank you for the clarity.
Also, I checked my oat milk-it says ‘calcium carbonate added.’ I switched to unsweetened, unfortified. It tastes like cardboard now, but my immune system is winning.
Acacia Hendrix
January 17, 2026 AT 10:46The pharmacokinetic interference between polyvalent cations and fluoroquinolone tetracyclines is a well-documented phenomenon in the literature-see J Clin Pharmacol 2018;58(4):456–463. The formation of chelate complexes via divalent metal ion coordination reduces bioavailability by orders of magnitude. This isn’t anecdotal-it’s physicochemical law.
Moreover, the FDA’s 2023 update to the antimicrobial stewardship guidelines explicitly mandates temporal separation for class-specific interactions. The 2-hour window for tetracyclines is insufficient for high-dose regimens; 3–4 hours is evidence-based. And let’s not forget the role of gastric pH modulation by calcium in altering dissolution kinetics.
It’s not ‘just dairy.’ It’s the ionic environment. Your almond milk? It’s a calcium bomb. Your ‘I’ve been fine for years’ narrative? That’s survivorship bias. You’re lucky.
Jesse Ibarra
January 18, 2026 AT 23:01So let me get this straight-you’re telling me I can’t have my morning latte with oat milk and my antibiotics? Who died and made you the Antibiotic Pope? I’m not a lab rat. I’m a human being with a life. You want me to schedule my yogurt like a NASA launch? Grow up.
I’ve been on cipro for a UTI and I ate a whole wheel of brie. Guess what? I’m fine. The bacteria didn’t win. I did. And I’m not apologizing for enjoying food.
Also, ‘calcium-fortified’ means it’s added. So what? Your body’s got a liver, a kidney, and a gut. They’re not broken. Stop treating yourself like a fragile robot.
Randall Little
January 20, 2026 AT 05:14So… if I take my antibiotic with water, then drink a smoothie with almond milk two hours later, I’m good? Or is that like, still a ‘bioavailability sabotage’? Because I’m starting to think this is just a conspiracy to sell more expensive XR pills.
Also, why does no one talk about how the FDA approved Cipro XR specifically to make people pay more? Like, the generic works fine-if you just don’t eat cheese. But hey, if you want to be a hero, go ahead and pay $200 for a pill that does the same thing.
And can we talk about how 43% of patients never got instructions? That’s not the patient’s fault. That’s the doctor’s. You’re blaming the victim.
jefferson fernandes
January 21, 2026 AT 03:09Let’s all take a breath. This is important, but it’s not a moral test. If you accidentally had yogurt with your pill once-don’t panic. Just be more careful next time.
But if you’re on a long course-like for Lyme or a chronic infection-timing matters. I’ve seen people relapse because they thought ‘it’s just dairy.’ It’s not. It’s chemistry. And chemistry doesn’t care how ‘natural’ you think you are.
Use a timer. Set a reminder. Write it on your fridge. This isn’t hard. You don’t need to be a scientist. Just be consistent.
And if you’re worried about your plant milk? Check the label. If it says ‘calcium added,’ treat it like milk. Simple.
Also-thank you to the pharmacist who actually told you this. They’re the real heroes.
Diana Campos Ortiz
January 21, 2026 AT 18:33i just took doxy this morning and i had oat milk in my coffee… oh no. 😅
but i read this post right after so now i know!! i’m switching to water for the next few days. and i’m gonna set a phone reminder for ‘no dairy for 3 hrs’
thank you for writing this. i didn’t know any of this. my doctor just said ‘take it on empty stomach’ and i thought that meant no breakfast, not no almond milk.
also, i just checked my almond milk-yep, calcium carbonate. guess i’m drinking plain water with my meds now. 🫖
John Tran
January 23, 2026 AT 08:04Think about it-this isn’t just about antibiotics. It’s about how we’ve been trained to treat our bodies like machines that need perfect inputs. We’re not machines. We’re messy, emotional, biological organisms that eat yogurt because it’s comforting. We take pills because we’re scared. We don’t need more guilt. We need compassion.
Yes, calcium binds. Yes, absorption drops. But your body isn’t a test tube. It adapts. It compensates. You’ve survived 30 years of bad sleep, coffee, sugar, and stress-do you really think one yogurt is going to break you?
And if you’re still worried? Talk to your doctor. Don’t let Reddit turn your healthcare into a cult. You’re not failing. You’re human.
Also, I once took cipro with a slice of pizza. I didn’t die. I lived. And I’m still here. Maybe the real superbug… is fear.
Angel Tiestos lopez
January 23, 2026 AT 15:02Bro. I took cipro with a smoothie. I didn’t die. I went hiking. I danced. I laughed. 😎
Maybe the real problem is that we’ve turned medicine into a ritual. Like, ‘you must wait 4 hours’ like it’s a sacred incantation. What if… your body knows what to do?
Also, I’ve had 3 UTIs. This was the first time I read about dairy. Why didn’t my doctor say this? 🤔
Maybe we need better doctors. Not more rules.
Alan Lin
January 24, 2026 AT 00:05As a former ER nurse, I’ve seen patients come in with recurrent infections because they took their antibiotics with milk, yogurt, or even calcium-fortified orange juice. It’s not speculation. It’s clinical reality.
One patient-a 72-year-old woman with a kidney infection-was on cipro. She drank a glass of calcium-fortified almond milk every morning with her pill. Her infection kept coming back. We found out when her daughter mentioned her ‘healthy smoothie habit.’
We told her to stop. She did. Infection cleared in 48 hours.
This isn’t about being perfect. It’s about being informed. If your doctor didn’t tell you, ask. If your pharmacist didn’t mention it, ask again. Your health is worth it.
And yes-plant milks with added calcium? Same rules. Same chemistry. Same risk.
Pankaj Singh
January 25, 2026 AT 16:50Wow. Another ‘dairy = antibiotic killer’ myth. Let’s see the actual pharmacokinetic data. What’s the AUC reduction? What’s the Cmax? What’s the statistical significance? You’re citing ‘studies’ like they’re gospel, but you’re not even naming them.
And why is doxycycline ‘less affected’? Because its binding constant to calcium is 10x lower than tetracycline. That’s basic chemistry. But you’re treating it like it’s the same.
Also, 22% of UTI failures due to dairy? Source? I’ve read every paper on this. That number is made up. You’re fearmongering to sell more expensive meds.
And don’t get me started on ‘superbugs’-antibiotic resistance is from overprescribing, not yogurt. Stop blaming the patient.
Robin Williams
January 26, 2026 AT 04:56Hey, I’m not perfect. I took my doxy with a cheese sandwich once. Felt like a rebel. 😎
But then I realized-I’m not fighting bacteria. I’m fighting laziness. So now I set a timer. I drink water. I wait. I win.
It’s not about being perfect. It’s about being intentional.
You don’t have to be a scientist. Just be a little more aware. Your future self will thank you.
Also-yes, your oat milk might be hiding calcium. Check the label. It’s not hard. 🙌
Adam Rivera
January 26, 2026 AT 18:46Just wanted to say-thank you for this. I’m from the Philippines and we eat a lot of yogurt and cheese here. I had no idea this was a thing. I’m on doxycycline right now and I’ve been eating cheese with my meals. I’m switching to water now.
Also, I checked our local oat milk-yep, calcium added. We’re gonna switch to plain rice milk now. Weird, but worth it.
Appreciate the clarity. This is the kind of info that actually saves lives.
Angel Tiestos lopez
January 27, 2026 AT 10:14Wait, so if I take my antibiotic at 7 a.m., and I have yogurt at 1 p.m., that’s fine? Or do I need to wait 6 hours? 🤔
Also, what if I take it at night? Can I have yogurt for breakfast the next day?