Confidence Interval: What It Is and Why It Matters in Medical Research
When you see a study saying a new drug lowers blood pressure by 10 mmHg, you might think that’s the exact number. But what if the real effect is 5 mmHg? Or 15? That’s where a confidence interval, a range of values that likely contains the true effect of a treatment based on sample data. Also known as CI, it helps you understand how precise a study’s findings really are. Unlike a single number, a confidence interval gives you a band — say, 7 to 13 mmHg — showing the range where the true result probably hides. This isn’t just math jargon. It’s how doctors and regulators decide if a drug works well enough to approve, or if a study’s results are too shaky to trust.
Confidence intervals are everywhere in medicine. They show up in studies about clinical trials, structured tests that compare new treatments to existing ones or placebos, like those for antidepressants or blood pressure meds. If a trial says a new pill reduces PTSD nightmares by 40% with a 95% confidence interval of 25% to 55%, you know the effect is likely real — and strong. But if the interval is 5% to 75%, that’s a red flag. The result could be barely noticeable or wildly effective. That’s why you can’t trust a study just because it says "statistically significant." That term often just means the p-value, a number that tells you how likely the result happened by random chance is below 0.05. But a tiny, useless effect can still get a low p-value if the sample size is huge. Confidence intervals cut through that noise. They show you the size of the effect, not just whether it exists.
Even more important, confidence intervals help you spot when a drug’s risks might outweigh its benefits. Take a medication that reduces stroke risk by 1% with a confidence interval of -0.5% to 2.5%. That negative number at the bottom means the drug might actually increase stroke risk for some people. Without seeing the full range, you’d miss that danger. That’s why regulators like the FDA look at confidence intervals — not just p-values — when reviewing new drugs. And when you’re reading about generic switching, genetic testing, or drug interactions, the same logic applies. If a study claims generics work just as well as brand names, but the confidence interval for effectiveness is wide and includes zero, you can’t be sure.
You’ll find confidence intervals in nearly every post here. From the safety of clozapine monitoring to the real impact of bepotastine eye drops, from the effectiveness of prazosin for PTSD nightmares to the true benefit of fiber for gut health — these studies don’t just give you numbers. They give you ranges. And understanding those ranges is the difference between making informed choices and being misled by flashy headlines. Below, you’ll see how these concepts show up in real medical research — and how to read them so you know what’s solid, what’s shaky, and what you should ask your doctor about.
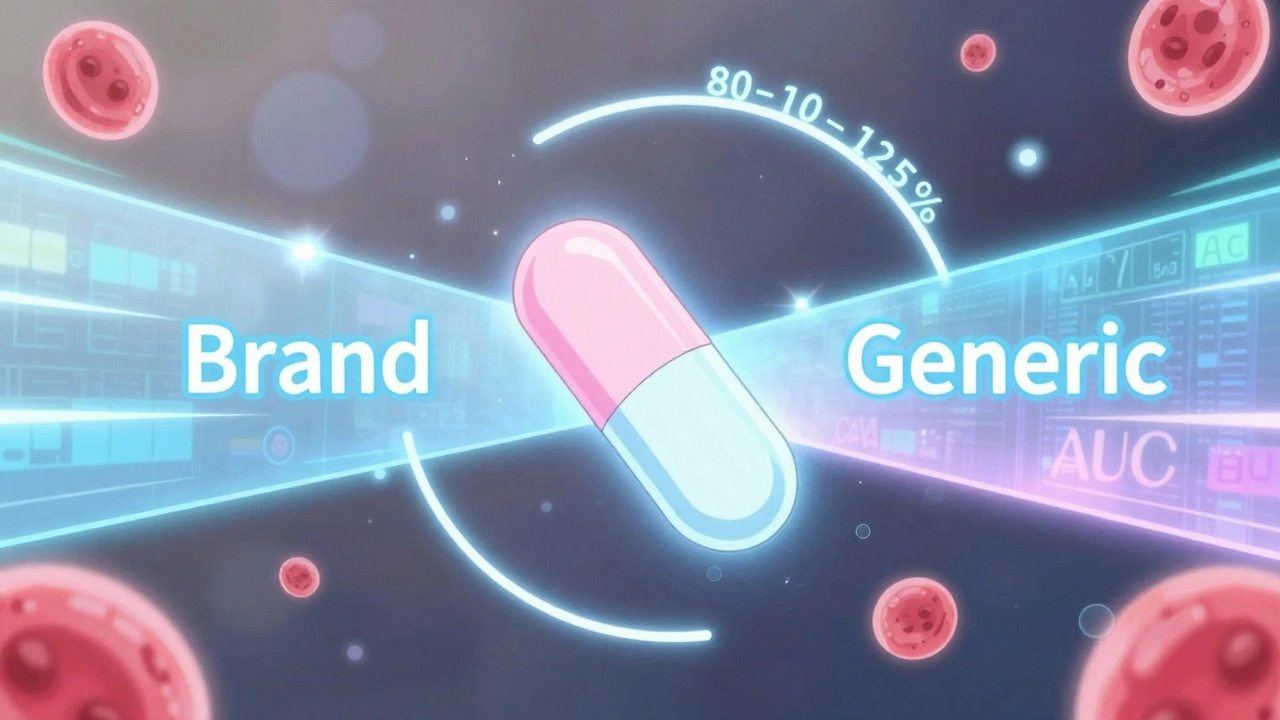
The 80-125% Rule: Understanding Bioequivalence Confidence Intervals for Generic Drugs
The 80-125% rule ensures generic drugs are absorbed the same way as brand-name versions. It's based on pharmacokinetic data, not drug content, and is used globally to approve safe, affordable generics.
December 1 2025