80-125 Rule: What It Means for Generic Drug Approval and Patient Safety
When you switch from a brand-name drug to a generic, you expect the same results—same relief, same side effects, same safety. That’s where the 80-125 rule, a FDA-standard bioequivalence threshold used to approve generic medications. Also known as bioequivalence range, it ensures that the amount of drug your body absorbs falls within 80% to 125% of the brand-name version. This isn’t a suggestion—it’s a legal requirement for generics to be sold in the U.S. If a generic drug doesn’t meet this range, it can’t be approved. Simple as that.
But here’s the catch: not all drugs play nice with this rule. For medications with a narrow therapeutic index—like warfarin, lithium, or thyroid hormones—even a small difference in absorption can cause serious harm. That’s why the FDA, the U.S. agency responsible for regulating drugs and ensuring public safety. Also known as Food and Drug Administration, it requires extra testing for these drugs. You’ll see this in posts about monitoring your health after switching to generics, or why clozapine and other high-risk meds need special oversight. The 80-125 rule is the baseline, but for some drugs, the FDA demands even tighter control.
The rule also explains why some people notice changes when they switch generics—even if both are labeled the same. Different manufacturers use different fillers, coatings, or release methods. These aren’t active ingredients, but they can affect how fast the drug gets into your blood. That’s why posts on bupropion side effects or SSRI switches often mention unexpected reactions: it’s not always the drug itself, but how your body handles the specific version you got. The 80-125 rule allows for this variation, but it doesn’t guarantee identical experience for everyone.
And what about false advertising in generics? If a company claims their generic is "identical" to the brand, they’re not lying under the 80-125 rule—but they’re oversimplifying. It’s not about being identical. It’s about being equivalent in effect. The therapeutic equivalence, the clinical outcome when two drugs produce the same effect in patients. Also known as bioequivalence, it is what matters, not chemical twins. That’s why posts on drug safety, REMS programs, and switching antidepressants all tie back to this same idea: your body responds to results, not labels.
If you’ve ever wondered why your doctor asks you to stick with one generic brand, or why some pharmacies won’t substitute certain meds without approval, now you know. The 80-125 rule is the invisible guardrail keeping millions of patients safe. But it’s not foolproof. That’s why monitoring your health after switching, understanding your drug metabolism through genetic testing, or checking for interactions with grapefruit juice all matter. These aren’t separate issues—they’re all part of the same system: making sure what you take does what it’s supposed to, every time.
Below, you’ll find real-world stories from people who’ve been affected by this rule—some because it worked perfectly, others because something slipped through. Whether you’re switching to a cheaper version of your blood pressure pill, managing RBD with clonazepam, or tracking side effects from duloxetine, the 80-125 rule is quietly shaping your experience. Know what it is. Know why it matters. And know when to speak up if something feels off.
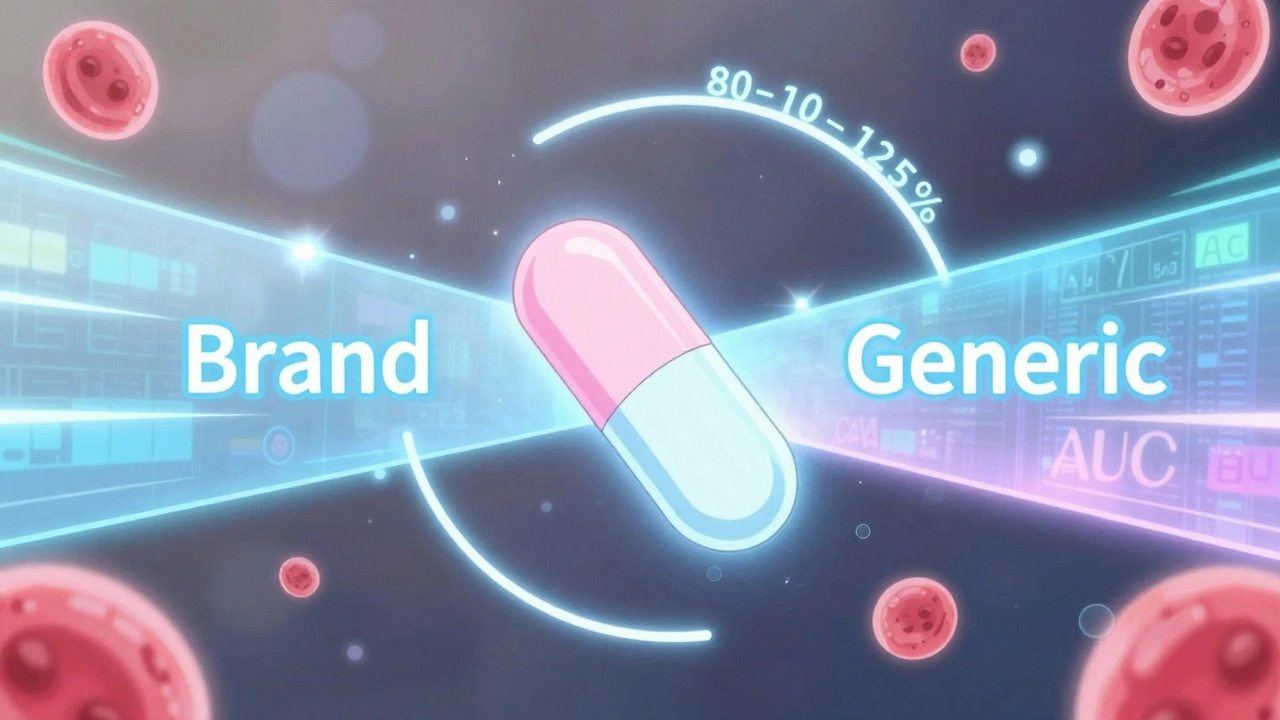
The 80-125% Rule: Understanding Bioequivalence Confidence Intervals for Generic Drugs
The 80-125% rule ensures generic drugs are absorbed the same way as brand-name versions. It's based on pharmacokinetic data, not drug content, and is used globally to approve safe, affordable generics.
December 1 2025