When a child shows signs of spasticity is a muscle‑tone disorder that causes stiffness, involuntary contractions, and limited movement, parents often feel unsure where to start. The reality is that early detection, tailored interventions, and a solid home plan can dramatically improve a child’s comfort and functional ability. Below you’ll find the core steps you need to take - from spotting red flags to choosing the right therapy - all explained in plain language.
Key Takeaways
- Spot early signs of spastic muscle states such as tightness, abnormal postures, or difficulty with voluntary movements.
- Get a formal assessment from a specialist; tools like the Modified Ashworth Scale help quantify severity.
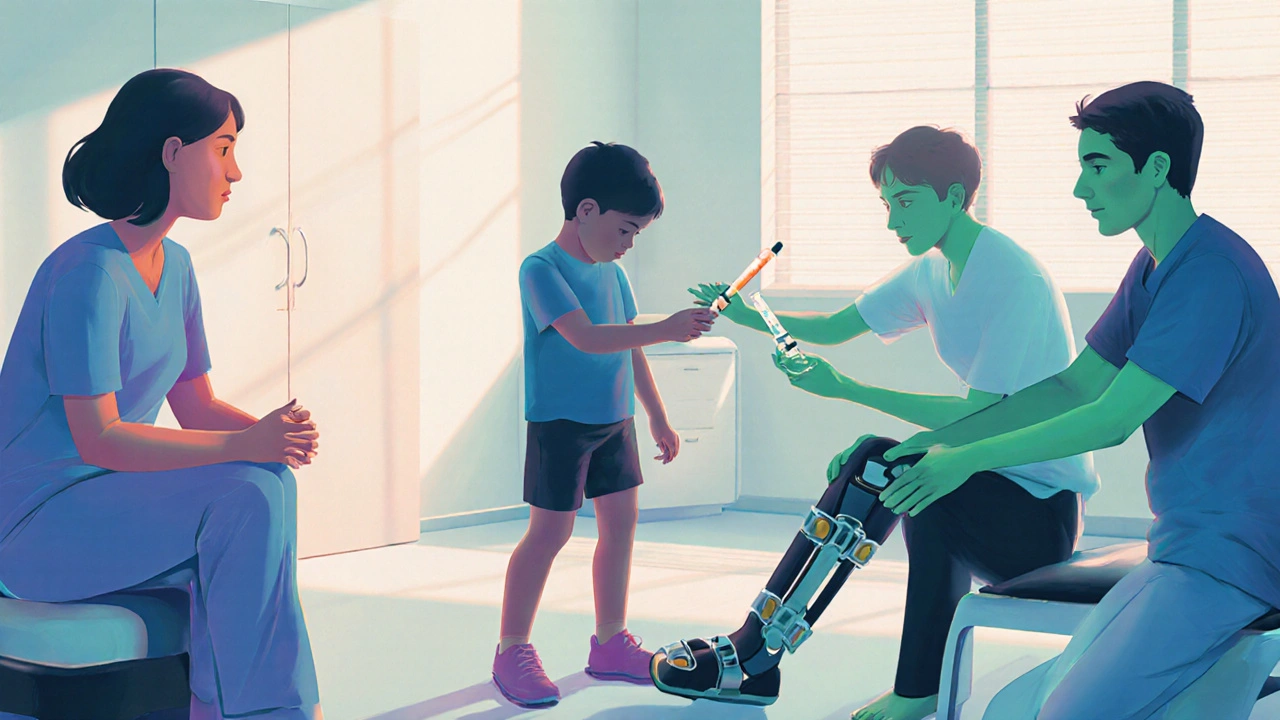
- Combine therapies - stretching, physical therapy, botulinum toxin, and orthotics - for the best functional gains.
- Maintain a consistent home‑exercise routine; consistency beats intensity.
- Tap into community resources and support networks to ease emotional and logistical burdens.
Understanding Spastic Muscle States in Children
Spasticity isn’t a disease in itself; it’s a symptom that often stems from brain or spinal‑cord injuries. The most common diagnosis linked to childhood spasticity is Cerebral Palsy (a group of permanent movement disorders caused by early brain damage. However, post‑traumatic brain injury, stroke, or genetic conditions can also produce similar muscle tone issues. The hallmark is hyper‑tonicity: muscles stay partially contracted even when the child tries to relax, leading to contractures, pain, and reduced mobility.
How Professionals Diagnose the Problem
Diagnosis begins with a thorough history and physical exam. Pediatric neurologists or physiatrists often use standardized tools such as:
- The Modified Ashworth Scale - rates resistance during passive movement from 0 (no increase) to 4 (rigid).
- The Gross Motor Function Measure (GMFM) - tracks functional abilities across lying, sitting, crawling, and walking.
- Instrumented gait analysis - captures walking patterns with motion‑capture cameras.
Imaging (MRI or CT) may be ordered to pinpoint the underlying lesion, but the clinical exam remains the cornerstone. Early, accurate grading helps clinicians map the most effective treatment pathway.
Core Treatment Options and When to Use Them
There’s no one‑size‑fits‑all answer. Most children benefit from a combination of approaches, each addressing a different aspect of the problem.
| Treatment | Invasiveness | Typical Duration of Effect | Best Age Range | Primary Benefit |
|---|---|---|---|---|
| Physical Therapy | Non‑invasive | Continuous (requires ongoing sessions) | All ages | Improves strength, flexibility, and motor control |
| Botulinum Toxin Injections | Minimally invasive | 3‑6 months | 2‑12 years (targeted muscles) | Reduces focal muscle tone, allowing better stretching |
| Orthopedic Surgery | Highly invasive | Permanent (unless complications) | Often after 4‑6 years when contractures stabilize | Corrects bone deformities, releases tight tendons |
| Assistive Devices | Non‑invasive | Ongoing (adjusted as child grows) | All ages | Supports posture, improves gait efficiency |
| Occupational Therapy | Non‑invasive | Continuous | All ages | Enhances daily‑living skills and fine‑motor function |
Physical Therapy: The Foundation
Physical Therapy (a specialized program focusing on movement, strength, and flexibility is usually the first line of defense. A licensed pediatric PT will design a routine that includes:
- Passive stretching of affected muscle groups (e.g., hamstrings, gastrocnemius).
- Active‑assisted exercises to promote voluntary control.
- Task‑specific gait training using treadmills or over‑ground walking.
- Proprioceptive and balance activities to improve postural stability.
Consistency is key. Sessions three times a week for the first six months, followed by a maintenance schedule, yield measurable gains on the GMFM scores. Home‑based practice should mirror clinic drills, but keep each stretch under 30 seconds and repeat 3‑5 times per muscle.
Targeted Botulinum Toxin Injections
When spasticity is focal-say, tight calf muscles that prevent proper foot clearance-Botulinum Toxin Injections (a neurotoxin that temporarily blocks nerve signals to the muscle can provide a therapeutic window. The procedure is performed under mild sedation or local anesthesia, and the effect typically lasts 3-6 months.
Key points for parents:
- Expect initial soreness for 1‑2 days.
- Combine with aggressive stretching and PT during the effect window.
- Repeat injections cautiously to avoid muscle atrophy.
Studies from 2023‑2024 show that children who receive botulinum toxin plus PT improve walking speed by up to 20% compared with PT alone.
Orthopedic Surgery: When Structural Change Is Needed
Chronic spasticity can lead to fixed contractures or bone deformities (e.g., tibial torsion). Orthopedic Surgery (procedures such as tendon lengthening, osteotomy, or joint realignment addresses these issues.
Pre‑operative planning involves:
- Radiographic assessment of bone alignment.
- Functional evaluation to determine which joints limit mobility.
- Coordination with the rehab team for post‑op therapy.
Post‑surgery, intensive PT for 6‑12 weeks is essential to maintain the new range and prevent re‑tightening.
Assistive Devices and Orthoses
Braces, ankle‑foot orthoses (AFOs), and walking aids are Assistive Devices (non‑invasive tools that support alignment and improve gait mechanics. A well‑fitted AFO can prevent foot drop, reduce energy expenditure, and allow a child to walk longer distances.
Things to watch for:
- Fit checks every 3-4 months as the child grows.
- Skin integrity - look for redness or breakdown.
- Comfort - the child should be able to sit and stand without pain.
Stretching Exercises and Home Programs
Simple Stretching Exercises (slow, sustained movements that lengthen tight muscles are the backbone of daily care. A typical routine might include:
- Supine hamstring stretch - hold 20‑30 seconds, repeat 3 times per leg.
- Standing calf stretch using a step - same timing.
- Passive hip abduction stretch with a therapist or caregiver assistance.
Integrate these into playtime; for example, turning a stretch into a “touch‑the‑toes” game keeps the child engaged. Consistency-twice daily-outperforms occasional marathon sessions.
Occupational Therapy: Fine Motor and Daily Living
While PT focuses on large‑muscle groups, Occupational Therapy (therapy that targets hand function, self‑care, and adaptive skills helps children manage everyday tasks. OT strategies include:
- Adaptive utensils for feeding.
- Sensory integration activities to reduce hyper‑reactivity.
- Fine‑motor drills such as bead threading or play‑dough shaping.
When combined with PT, children often show accelerated progress in school participation and independence.
Emotional and Social Support for Families
Dealing with spastic muscle states can be overwhelming. Parents should consider:
- Joining local support groups-many hospitals run monthly parent meet‑ups.
- Accessing counseling services to manage stress and anxiety.
- Leveraging online forums dedicated to cerebral palsy and spasticity management.
Research from 2022 demonstrates that families with strong peer networks report better adherence to therapy schedules and higher overall quality of life.
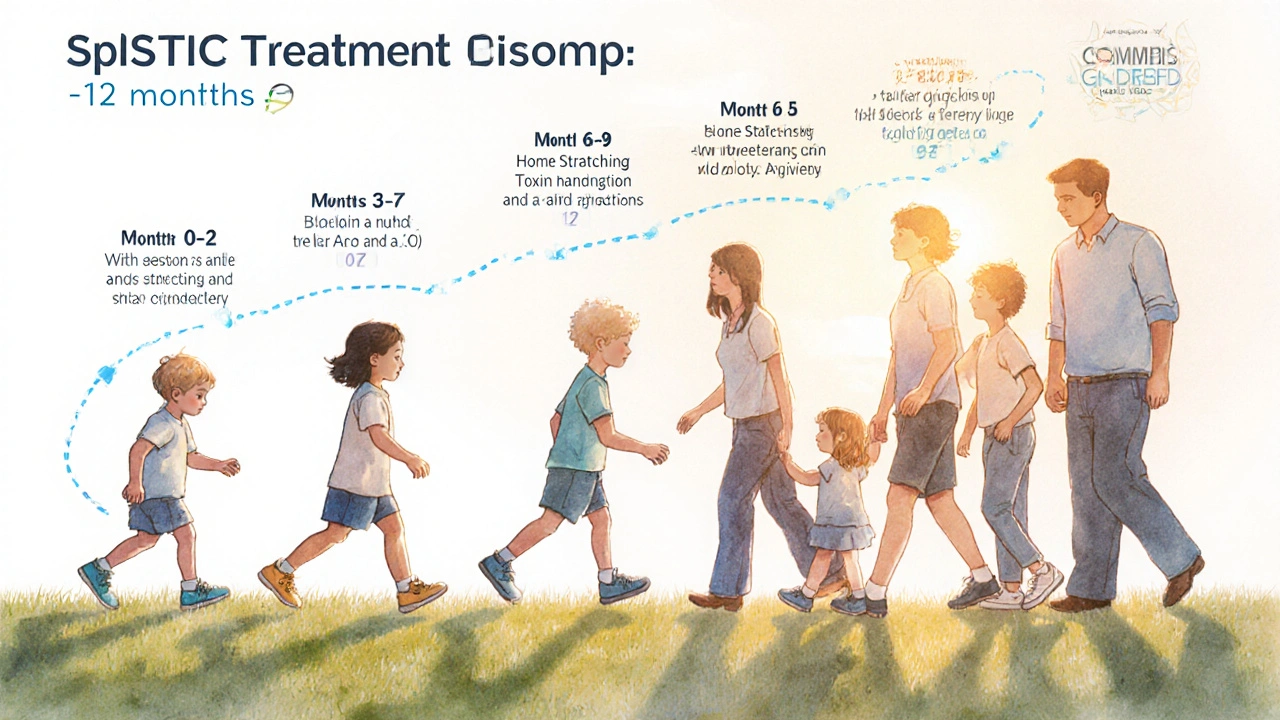
Putting It All Together: A Sample 12‑Month Roadmap
Below is a realistic timeline that many families follow. Adjustments may be needed based on the child’s response.
- Month 0‑2: Obtain diagnosis, baseline assessments (Modified Ashworth, GMFM), and start PT twice weekly.
- Month 3‑5: Introduce daily home stretching, evaluate need for botulinum toxin; if indicated, schedule first injection.
- Month 6‑9: Fit AFOs or other orthoses, continue PT and add OT sessions for fine‑motor skills.
- Month 10‑12: Re‑assess muscle tone; consider orthopedic consult if contractures persist despite conservative care.
Regular check‑ins with the multidisciplinary team keep the plan flexible and focused on the child’s evolving goals.
Frequently Asked Questions
What are the earliest signs of spastic muscle problems?
Parents often notice tightness in the calves or arms, a preference for one side when crawling, or difficulty straightening a limb after a nap. Early referral to a pediatric neurologist can confirm if spasticity is present.
Is botulinum toxin safe for young children?
When administered by an experienced pediatric specialist, the dosage is weight‑based and has been shown to be safe. Side effects are usually mild, such as temporary soreness or bruising at the injection site.
How often should we do home stretching?
Twice daily, holding each stretch for 20‑30 seconds and repeating 3-5 times per muscle group, yields the best results. Incorporate the routine into play or bedtime rituals to make it stick.
When is orthopedic surgery considered?
Surgery is typically explored when contractures become fixed, limiting function despite aggressive PT and botulinum toxin. Ages 4‑8 are common windows, but the decision is individualized.
Can a child outgrow spasticity?
Spasticity itself may lessen as the nervous system matures, but many children retain some degree of tone abnormality. Ongoing therapy helps maximize functional independence regardless of changes in tone.


Timothy Javins
October 13, 2025 AT 19:31Honestly, the guide sounds like a one‑size‑fits‑all manual, but every child's spasticity is unique, so blanket recommendations can be misleading. While early detection is crucial, the emphasis on standardized scales sometimes overshadows the need for individualized observation. Parents might feel pressured to chase every assessment instead of listening to their child's subtle cues. The article also glosses over the socioeconomic barriers many families face when accessing multidisciplinary care. In short, the “practical” label feels more aspirational than realistic.
Rajesh Kumar Batham
October 13, 2025 AT 19:36I get where you’re coming from, but the step‑by‑step layout can actually give families a solid starting point 😊. It breaks down a complex topic into bite‑size pieces, which is exactly what many parents need when they first hear the word “spasticity.” Plus, the resources listed at the end help bridge that gap between theory and real‑world help. So, while it’s not perfect, it’s definitely a useful launchpad. 🙌
Bill Gallagher
October 13, 2025 AT 19:41The comprehensive nature of this guide is, in my view, an exemplary synthesis of contemporary pediatric neurology, orthopaedic intervention, and rehabilitative strategy; it meticulously integrates diagnostic metrics such as the Modified Ashworth Scale and the Gross Motor Function Measure, thereby providing clinicians with a quantifiable framework that transcends anecdotal practice. Moreover, the inclusion of evidence‑based timelines, for instance the recommendation of bi‑weekly physiotherapy sessions for the initial six‑month period, aligns with longitudinal studies indicating measurable improvements in functional mobility and reduced contracture formation. It is also noteworthy that the article delineates the pharmacodynamics of botulinum toxin, specifying dosage considerations and the temporal window for adjunctive stretching-a nuance often omitted in layperson resources. The tabular comparison of treatment modalities, ranging from non‑invasive physical therapy to highly invasive orthopedic surgery, offers a clear hierarchy of intervention intensity, facilitating shared decision‑making among caregivers and multidisciplinary teams. In addition, the discussion of assistive devices such as ankle‑foot orthoses underscores the importance of biomechanical alignment in mitigating energy expenditure during ambulation. The emphasis on caregiver education, particularly the recommendation to integrate stretching into playtime, reflects an appreciation for behavioral adherence strategies rooted in pediatric occupational therapy literature. Furthermore, the guide’s acknowledgment of psychosocial support mechanisms, including peer‑led support groups and counseling services, highlights a holistic approach that addresses both physical and emotional dimensions of spasticity management. The systematic presentation of a twelve‑month roadmap provides a temporal scaffold that can be customized to individual response trajectories, thereby respecting the heterogeneity of spastic presentations. While the article is thorough, one might argue that it could benefit from a deeper exploration of emerging modalities such as selective dorsal rhizotomy, which, although invasive, has demonstrated long‑term efficacy in select cohorts. Additionally, the brief mention of intrinsic motivation techniques could be expanded to incorporate goal‑setting frameworks that have been validated in pediatric rehabilitation settings. The guide also appropriately cautions against over‑reliance on any single intervention, advocating for a multimodal regimen that synergizes pharmacologic, therapeutic, and orthotic strategies. In sum, the document serves as a valuable conduit between scientific evidence and practical application, embodying a model of patient‑centered care that is both rigorous and accessible.
Rajashree Varma
October 13, 2025 AT 19:46The guide does a great job of summarizing key steps and it feels very encouraging for families who might be overwhelmed. Its clear language and emphasis on consistency really help demystify the process. By laying out a roadmap it gives hope and direction without being overly technical. The tone stays positive and supportive which is exactly what caregivers need.
Sam Franza
October 13, 2025 AT 19:51Thanks for the solid overview.
Raja Asif
October 13, 2025 AT 19:56That “solid overview” ignores the fact that many of these protocols were developed in high‑income countries and simply don’t translate to our local realities where resources are scarce and cultural expectations differ.
Cynthia Sanford
October 13, 2025 AT 20:01i totally agree the guide is super helpful but remember to adapt it to ur kid’s vibe and dont stress if some steps feel tough at first, keep it chill and celebrate small wins!
Yassin Hammachi
October 13, 2025 AT 20:06Adapting the plan to a child’s daily rhythm really does make the difference; when therapy feels like a game rather than a chore, motivation naturally follows, and that’s where sustainable progress originates.
Brooks Gregoria
October 13, 2025 AT 20:11If we keep dissecting spasticity into boxes of scales and schedules, we risk turning a living, breathing child into a checklist; perhaps the real therapy lies in embracing the messiness of human development rather than forcing order upon it.
Sumit(Sirin) Vadaviya
October 13, 2025 AT 20:16While the sentiment captures the complexity of caring for a child with spasticity, structure does provide a necessary scaffold that can prevent overwhelm 😊; a balanced approach that marries flexibility with evidence‑based milestones often yields the most compassionate care 🌟.
lindsey tran
October 13, 2025 AT 20:21yeah, i feel that too!! it's like walking a tightrope between chaos and control, and every little victory feels like a fireworks show in the night sky!! 🎆
Krishna Sirdar
October 13, 2025 AT 20:26Every family’s journey is unique, so sharing tips, listening with empathy, and offering practical ideas can help each other grow stronger together.