GERD vs Heart Attack Chest Pain Checker
Answer the following questions to help determine if your chest pain is more likely GERD-related or potentially cardiac:
Quick Take
- GERD can mimic heart‑related chest pain, but the triggers and timing differ.
- Burning pain after meals, especially when lying down, often points to acid reflux.
- A sudden crushing pressure, radiating to the left arm or jaw, demands emergency care.
- Red‑flag signs include shortness of breath, sweating, or loss of consciousness.
- Managing lifestyle, weight, and medication can reduce GERD‑related discomfort.
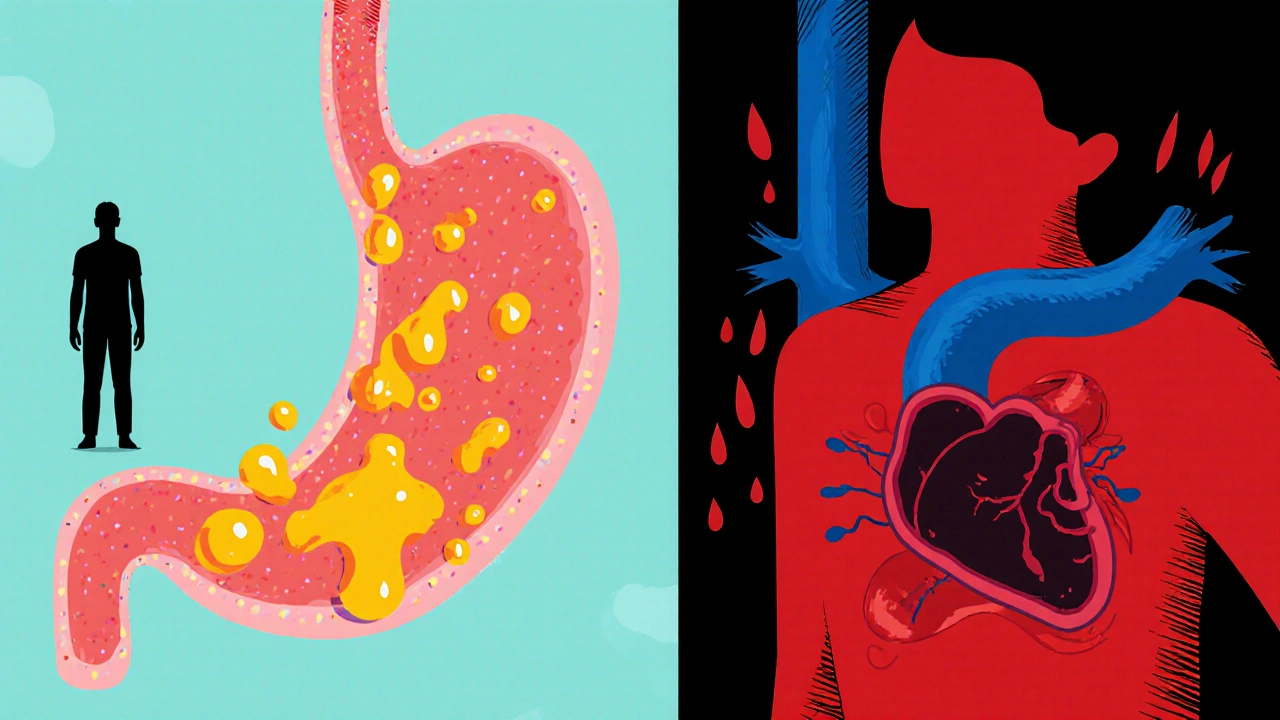
When you feel a tightness in your chest, the mind instantly jumps to the worst‑case scenario: a heart attack. But not every pang is cardiac. Gastroesophageal reflux disease (GERD) is a chronic condition where stomach acid frequently flows back into the esophagus, the tube that connects your mouth to your stomach. This backflow, also called acid reflux, can produce a burning sensation that many call heartburn. Sometimes, the pain spreads to the chest, making it hard to tell if the heart or the gut is the culprit.
Understanding the anatomy helps. The esophagus is a muscular tube that pushes food toward the stomach is protected by the lower esophageal sphincter (LES). When the LES relaxes inappropriately, acid escapes, irritating the lining. This irritation can trigger the nerves that also serve the heart, creating a confusing overlap of sensations.
How GERD Causes Chest Pain
Three main mechanisms link GERD to chest discomfort:
- Direct acid irritation: The acid burns the esophageal lining, producing a burning or pressure‑like feeling behind the breastbone.
- Esophageal spasm: The esophagus may contract forcefully as a reaction to acid, mimicking the squeezing sensation of angina.
- Referred pain: Nerve pathways that serve both the esophagus and the heart can carry pain signals to the same chest area.
While these episodes are uncomfortable, they seldom threaten life. However, distinguishing them from true cardiac events is crucial because the stakes are dramatically different.
Typical Features of GERD‑Related Chest Pain
GERD chest pain tends to follow a pattern. Look for these clues:
- Timing: Pain often starts after a large or fatty meal, or when you lie down or bend over.
- Location: The burning sensation is usually centered behind the breastbone (retrosternal) and may travel up the throat.
- Quality: Described as a “burn,” “sour taste,” or a “tight band” rather than a crushing pressure.
- Relief: Antacids, upright posture, or chewing gum can quickly ease the discomfort.
- Associated symptoms: Regurgitation, sour taste, hoarseness, or chronic cough.
When the pain meets most of these criteria, GERD is a likely suspect.
Red‑Flag Signs That It Might Be More Than Heartburn
Not all chest pain is benign. Certain features should push you to seek immediate medical attention:
- Sudden, crushing pressure that lasts more than a few minutes.
- Radiation to the left arm, jaw, neck, or back.
- Accompanying shortness of breath, cold sweats, nausea, or light‑headedness.
- Pain that occurs at rest, especially during sleep.
- History of heart disease, high blood pressure, high cholesterol, or diabetes.
If any of these appear, call emergency services. Time is muscle when the heart is involved.
Comparing GERD Chest Pain and Cardiac Chest Pain
| Aspect | GERD‑Related Pain | Cardiac Pain (Angina/Heart Attack) |
|---|---|---|
| Typical Triggers | After meals, lying down, bending over | Physical exertion, emotional stress, cold weather |
| Pain Quality | Burning, sour, pressure‑like, improves with antacids | Heavy, crushing, squeezing, does not improve with antacids |
| Radiation | Often limited to chest and throat | Arm, jaw, neck, back, sometimes teeth |
| Associated Symptoms | Regurgitation, hoarseness, chronic cough | Shortness of breath, sweating, nausea, dizziness |
| Response to Position | Improves when upright | No change or worsens when lying flat |
| Diagnostic Tests | Upper endoscopy, pH monitoring, trial of PPIs | ECG, cardiac enzymes, stress test, angiography |
When to See a Doctor
Even if the pain seems typical of GERD, a professional evaluation is wise when:
- Symptoms persist despite over‑the‑counter antacids.
- You need to use medication more than twice a week.
- Night‑time pain wakes you up regularly.
- There’s unexplained weight loss or difficulty swallowing.
- Red‑flag cardiac signs appear, however mild they seem.
Your doctor may order an upper endoscopy to look for erosive esophagitis or more serious complications like Barrett's esophagus a condition where the esophageal lining changes due to chronic acid exposure, increasing cancer risk. Early detection helps prevent progression.
Managing GERD‑Related Chest Pain
Three pillars guide treatment: lifestyle tweaks, medication, and, when needed, procedures.
Lifestyle Adjustments
- Eat smaller meals: Large meals stretch the stomach and increase pressure on the LES.
- Avoid trigger foods: Spicy dishes, citrus, chocolate, caffeine, alcohol, and fatty foods.
- Stay upright after eating: Wait at least two to three hours before lying down.
- Elevate the head of the bed: A 6‑inch wedge reduces nighttime reflux.
- Quit smoking: Nicotine relaxes the LES.
Medications
First‑line therapy usually involves proton pump inhibitors (PPIs) drugs that block the stomach’s acid‑producing pumps, providing long‑lasting relief. Common options include omeprazole, esomeprazole, and lansoprazole. For occasional symptoms, H2‑blockers like ranitidine (where available) or antacids can be sufficient.
Procedural Options
When medication and lifestyle changes fail, procedures such as laparoscopic fundoplication (tightening the LES) or endoscopic radiofrequency treatment may be considered. These are generally reserved for severe, refractory cases.
Quick Self‑Check: Is Your Chest Pain Likely GERD?
- Did the pain start after a meal or when you lay down?
- Does it feel like burning or a sour taste in your throat?
- Do antacids or a change in position make it better?
- Are you missing any red‑flag cardiac symptoms (arm pain, sweating, dizziness)?
If you answered “yes” to the first three and “no” to the last, GERD is a strong possibility. Still, when in doubt, err on the side of caution and get evaluated.
Key Takeaways
- GERD can produce chest pain that looks like heart disease, but the triggers, relief methods, and associated symptoms differ.
- Watch for red‑flag signs-sudden crushing pressure, radiation to the arm or jaw, shortness of breath-and seek emergency care immediately.
- Lifestyle changes and PPIs control most GERD cases; endoscopy helps rule out complications.
- Never ignore persistent or worsening chest pain; a brief assessment can save a life.

Frequently Asked Questions
Can GERD cause a heart attack?
No. GERD itself does not damage the heart. However, the chest pain it causes can feel similar to a heart attack, which is why distinguishing the two is essential.
How long should I try over‑the‑counter antacids before seeing a doctor?
If symptoms persist after a week of regular antacid use, or if you need them more than twice a week, schedule a medical evaluation.
Is it safe to take PPIs long‑term?
Short‑term PPI therapy is safe for most adults. Long‑term use may increase risks of vitamin B12 deficiency, bone fractures, and infections, so discuss duration with your doctor.
What tests confirm GERD as the cause of chest pain?
Upper endoscopy, 24‑hour pH monitoring, and esophageal manometry can objectively measure acid exposure and LES function.
When should I call emergency services for chest pain?
Call 911 immediately if the pain is sudden, crushing, lasts more than a few minutes, radiates to the arm/jaw, or is accompanied by sweating, nausea, or shortness of breath.


Jennifer Romand
October 2, 2025 AT 22:22Honestly, the whole GERD vs heart‑attack debate feels like a melodramatic soap opera where everyone pretends they’ve never heard of the simple rule: if it’s crushing and radiates, call 911.
Kelly kordeiro
October 5, 2025 AT 05:56It is an undeniable truth that the human chest, being the central hub of both corporeal vigor and existential trepidation, serves as the canvas upon which myriad pathophysiological narratives are painted, each vying for the attention of the discerning observer. In the grand tapestry of gastrointestinal and cardiovascular interplays, one must first acknowledge the elegant orchestration of the lower esophageal sphincter, whose occasional rebellion against its own duties precipitates the acid reflux we so colloquially term "heartburn". Yet, let us not be beguiled by mere nomenclature, for the burning sensation that climbs the esophagus often masquerades as a cardiac omen, leading even the most erudite among us astray. The temporal relationship between a lavish, fatty banquet and the subsequent emergence of retrosternal discomfort is, by all accounts, a hallmark of gastro‑esophageal reflux disease, a condition both pervasive and, fortunately, amenable to lifestyle modification and pharmacologic intervention. Conversely, the sudden onset of a pressure-like, crushing pain, unbidden by the hour of the post‑prandial period, and which radiates with disquieting fidelity to the left arm, jaw, or neck, is the clarion call of myocardial ischemia, demanding immediate medical attention. Moreover, the autonomic manifestations – diaphoresis, nausea, and a sense of impending doom – serve as the body's unapologetic alarm system, a siren that should never be ignored or dismissed as mere indigestion. The diagnostic armamentarium at our disposal, ranging from the humble over‑the‑counter antacid to the sophisticated coronary angiogram, provides a stratified approach to delineating these entities. While proton pump inhibitors can quell the acid assault on the esophageal mucosa, they are powerless against the vascular occlusion that characterizes an acute coronary syndrome. It is, therefore, incumbent upon both patient and practitioner to meticulously parse the symptomatology, observing the nuances of timing, quality, and associated features, lest we err on the side of complacency. In summation, the delineation between GERD‑induced chest discomfort and true cardiac pathology rests upon a careful appraisal of triggers, alleviating factors, and red‑flag signals; a discernment that can ultimately mean the difference between a routine clinic visit and a life‑saving emergency response.
Chris Fulmer
October 7, 2025 AT 13:29Great rundown! I think it’s helpful to remember that the timing of pain-after a big meal or when you’re lying down-often points toward reflux, while a sudden, crushing feeling out of nowhere leans toward the heart.
William Pitt
October 9, 2025 AT 07:09Exactly, Chris. It’s all about those clues. If antacids calm things down, you’re probably dealing with GERD. But never ignore radiating pain or sweating – that’s a red flag.
Jeff Hershberger
October 11, 2025 AT 14:42One must not be obtuse enough to think that the fire‑breathing demon of acid reflux could ever mimic the thunderous roar of a myocardial infarction; the latter is a beast of a different stripe.
Jesse Najarro
October 13, 2025 AT 08:22yeah its good info but i think people need to see doctor if they cant figure it out themselves
Dan Dawson
October 14, 2025 AT 17:42Know your heart.
Lawrence Jones II
October 16, 2025 AT 05:49TL;DR: If it burns after a burger 🍔 and eases when you sit up, it’s probably GERD. If it feels like an iron band crushing your chest and you’re sweaty, call 911 ⚡.
Robert Frith
October 17, 2025 AT 23:29Mate, I’m sick of people thinkin’ a bit of heartburn is an actual heart attack. Get your facts straight before you start panic‑selling vitamin C.
Albert Gesierich
October 19, 2025 AT 17:09Robert, just to be clear: GERD isn’t a cardiac event, but the symptoms can overlap. It’s crucial to differentiate the two based on triggers, relief, and accompanying signs.
Brad Tollefson
October 21, 2025 AT 05:16Albert, thanks for the clarification. It’s easy to get confused, especially when the pain is vague.
Paul van de Runstraat
October 22, 2025 AT 14:36Glad we’re all on the same page now-hopefully nobody ends up in the ER because they ignored the classic red‑flag signs.
Suraj Midya
October 24, 2025 AT 08:16Red flag signs are universal, regardless of where you live.
ashish ghone
October 26, 2025 AT 01:56Friends, remember that lifestyle changes-like eating smaller meals, avoiding late‑night snacks, and staying upright after eating-can dramatically reduce GERD‑related chest pain. 🍽️🛏️ And if you ever feel uncertain, don’t hesitate to reach out to a healthcare professional; early intervention is always better than regret.
steph carr
October 27, 2025 AT 18:36Exactly! Small tweaks can make a huge difference, and staying informed helps us all stay safe.
Vera Barnwell
October 29, 2025 AT 12:16While many of us trust mainstream medical advice, it's worth noting that some pharmaceutical companies downplay the long‑term risks of PPIs, subtly nudging patients into indefinite use. This can lead to hidden issues like calcium malabsorption, increased fracture risk, and even gut microbiome disruptions. One must stay vigilant, read the fine print, and consider natural alternatives where appropriate. The truth is, the medical establishment isn’t always your ally; they have vested interests that can cloud judgment and compromise patient safety. So, approach any medication with a healthy dose of skepticism and always ask for the data.
Dawn Midnight
October 30, 2025 AT 21:36Vera, while your concerns are noted, the statement about “pharmaceutical companies downplay risks” needs citation; otherwise it borders on misinformation.
frank hofman
November 1, 2025 AT 09:42Everyone’s got an opinion, but let’s not turn this into a conspiracy forum 🙄.
Dannii Willis
November 3, 2025 AT 03:22Appreciate the balanced discussion here-knowledge and caution go hand in hand.
Robyn Du Plooy
November 4, 2025 AT 21:02Totally agree! Quick self‑check tools are gold, but they aren’t a substitute for professional assessment when red‑flags appear.