Supplement & Medication Interaction Checker
This tool helps identify common interactions between dietary supplements and prescription medications. Remember: This is not a substitute for professional medical advice. Always consult your healthcare provider before making changes to your medications or supplements.
Why this matters
Over 77% of American adults take supplements, yet only about one-third tell their doctor. Many supplements can interact dangerously with medications, like St. John's wort with birth control or ginkgo biloba with blood thinners. Your care team needs to know what you're taking to keep you safe.
Enter Your Medications and Supplements
Results
Enter your medications and supplements to check for potential interactions.
Every year, millions of people in Australia and around the world take dietary supplements-vitamins, herbs, minerals, or extracts-thinking they’re harmless because they’re "natural." But here’s the hard truth: just because something comes from a plant or a bottle labeled "pure" doesn’t mean it’s safe to use without telling your doctor. In fact, some of the most dangerous drug interactions happen not with prescription pills, but with the supplements you didn’t think were worth mentioning.
What You’re Taking Might Be Hiding in Plain Sight
You might not even call it a supplement. Maybe you grab a garlic capsule for your cold, a ginkgo pill for memory, or St. John’s wort for low mood. You might take glucosamine for your knees or fish oil for heart health. These are all dietary supplements, and under Australian and U.S. regulations, they’re treated like food-not medicine. That means they don’t need to be proven safe or effective before hitting store shelves. The FDA doesn’t approve them. Neither does TGA in Australia. Manufacturers aren’t required to prove they work or that they won’t mess with your blood pressure meds, blood thinners, or antidepressants.And here’s the kicker: 77% of American adults take at least one supplement. In Australia, numbers are rising fast, with over 60% of adults using them regularly. Yet, studies show only about one-third of people tell their doctor. Why? Because they assume their doctor doesn’t care. Or they think, "It’s just a vitamin." But if you’re on warfarin and you start taking ginkgo biloba, you could bleed internally. If you’re on birth control and using St. John’s wort, you might get pregnant. These aren’t rare cases-they happen daily.
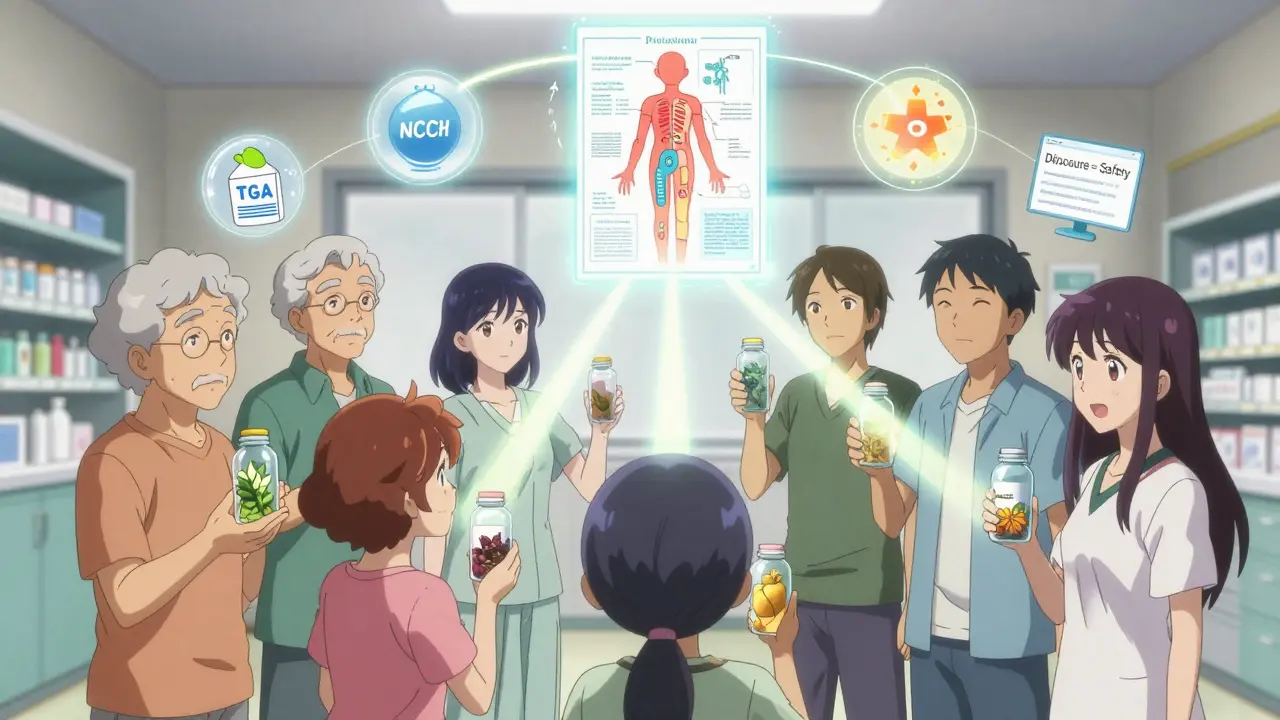
The Silent Gap in Communication
When you walk into a GP’s office, they ask about your medications. They check your prescriptions. They look for allergies. But how often do they ask: "What supplements are you taking?" The answer? Not often enough. Research shows that when doctors don’t ask directly, only 29% of patients volunteer the information. But when they do ask-clearly and without judgment-disclosure jumps to 72%.In Australia, disclosure rates are better than in the U.S. (around 68%), but they’re still far from perfect. Why? Because many doctors weren’t trained to talk about supplements. Medical schools in Australia and elsewhere spend less than 3 hours total on nutrition and natural products across four years of training. That’s not enough to build confidence. So they skip the question. And patients, sensing that the topic isn’t taken seriously, stay quiet.
But it’s not just about doctors. Patients also assume their pharmacist knows everything. Wrong. Most pharmacists don’t have access to your full supplement list unless you tell them. And if you buy supplements online-over 14% of sales are now online-you might not even know what’s in them. Labels can be misleading. One study found that 80% of supplements labeled as "ginseng" didn’t contain any actual Panax ginseng. Another had toxic levels of lead.
Real Risks, Real Consequences
Let’s get specific. Here are the supplements with the highest risk and lowest disclosure rates:- St. John’s wort: Reduces the effectiveness of 57% of prescription drugs-including antidepressants, birth control, and HIV meds. A viral TikTok video from a nurse showed a patient who got pregnant despite using birth control because of this herb.
- Ginkgo biloba: Thins the blood. Combine it with aspirin, warfarin, or even ibuprofen, and you risk brain or internal bleeding. A 2022 case study in the AMA Journal of Ethics described a patient who had a stroke after combining ginkgo with warfarin. She didn’t tell her doctor because she thought "it was just natural."
- Garlic and echinacea: Can interfere with HIV medications and immune suppressants used after transplants.
- Green tea extract: Linked to severe liver damage in some users. The FDA has issued multiple warnings.
- Glucosamine/chondroitin: Often taken by diabetics for joint pain. But it can raise blood sugar levels. If you’re on metformin, this could throw your whole regimen off.
The numbers don’t lie. In the U.S., 23,000 people end up in emergency rooms each year because of supplement reactions. In Australia, we don’t track it as closely, but the trend is clear: more people are using them, and more are getting hurt.
What You Need to Tell Your Care Team
You don’t need to be an expert. You just need to be honest. Here’s what to share:- The exact name: Say "Panax ginseng," not just "ginseng." "Turmeric extract" isn’t enough-say "curcumin 500mg daily."
- The dose and frequency: "I take 1,000 mg of fish oil twice a day."
- Why you’re taking it: "I take magnesium because I have trouble sleeping."
- Where you bought it: "I got it online from a brand called NutraVita."
Don’t wait for your annual checkup. Bring it up at every visit. If your doctor doesn’t ask, ask them: "Do you need to know about the supplements I’m taking?"
How Providers Are Starting to Catch Up
Change is happening. In Australia, some private hospitals now include supplement questions in admission forms. The TGA has started cracking down on false claims. The National Center for Complementary and Integrative Health (NCCIH) offers free training for clinicians-over 14,000 Australian and U.S. doctors have taken it. Electronic health records are finally updating: Epic Systems, the software used by most clinics, is rolling out a supplement module in mid-2024 that will flag dangerous interactions automatically.But the biggest shift isn’t technological-it’s cultural. Providers who ask open-ended questions like, "What are you using to support your health?"-not just "Are you taking any supplements?"-see far better results. One nurse in Sydney started asking: "What vitamins or natural products are you using that your pharmacist might not know about?" Disclosure in her practice doubled.
What You Can Do Right Now
You don’t need to wait for your doctor to ask. Take control. Here’s how:- Make a list: Write down every supplement you take, including brand, dose, and why. Keep it updated.
- Bring it to every appointment: Even if it’s just for a cold. Put it on your phone as a note. Print it out. Hand it to your doctor.
- Ask your pharmacist: They can check for interactions. Many pharmacies offer free reviews.
- Use trusted sources: Look up your supplement on the National Center for Complementary and Integrative Health (NCCIH) or the Therapeutic Goods Administration (TGA) website. Check for warnings.
- Don’t assume "natural" means safe: Just because it’s sold in a health food store doesn’t mean it’s harmless.
It’s Not About Trusting or Distrusting Supplements
It’s about communication. Supplements aren’t the enemy. Many people benefit from them-vitamin D for low sunlight, omega-3s for inflammation, magnesium for muscle cramps. But when they’re used without awareness, they become hidden risks.Think of your care team like a team of detectives. If you only give them half the clues, they can’t solve the case. Your blood pressure, your mood, your recovery after surgery-they all depend on knowing the full picture. That includes what’s in your medicine cabinet, your supplement drawer, and your daily routine.
So next time you’re at the clinic, don’t wait. Say it out loud: "I’m also taking [name]." It’s not a burden. It’s your safety.
Do I need to tell my doctor about every vitamin I take?
Yes. Even if it’s just a daily multivitamin or vitamin D. Some vitamins can interact with medications. For example, vitamin K can reduce the effect of blood thinners like warfarin. Vitamin C in high doses can interfere with certain cancer treatments. Your doctor needs the full picture to make safe decisions.
Can natural products cause serious side effects?
Absolutely. St. John’s wort can cause serotonin syndrome when mixed with antidepressants. Green tea extract has caused liver failure in some people. Kava has been linked to severe liver damage. Even common herbs like echinacea can trigger allergic reactions or interfere with immune-suppressing drugs after organ transplants. "Natural" doesn’t mean safe-it just means unregulated.
What if my doctor dismisses supplements as "just herbs"?
That’s a red flag. If your doctor doesn’t take your supplement use seriously, it’s time to find someone who does. The American Medical Association and the TGA both recommend routine screening for supplement use. A good provider will ask, listen, and check for interactions-not judge. You’re not overreacting; you’re protecting your health.
Are online supplements more dangerous?
Yes, often. Online supplements are less likely to be tested for purity or potency. A 2023 study found that 40% of supplements bought online contained unlisted ingredients-including prescription drugs, steroids, or heavy metals. Stick to reputable brands with third-party testing (look for USP, NSF, or ConsumerLab seals). If it’s sold on a random website with no reviews, assume it’s risky.
Should I stop taking supplements before surgery?
Yes, usually. Many supplements can interfere with anesthesia, increase bleeding risk, or affect blood pressure. Common ones to stop 1-2 weeks before surgery include garlic, ginkgo, fish oil, ginger, and green tea. Always ask your surgeon or anesthesiologist what to stop-and when. Don’t assume they’ll know.
How can I find out if my supplement interacts with my medication?
Use trusted databases like the Natural Medicines Database (available through many hospitals), the TGA’s website, or the National Center for Complementary and Integrative Health (NCCIH). Your pharmacist can also run a check. Never rely on Google or social media. A single interaction can be life-threatening.




Luke Trouten
February 14, 2026 AT 00:03It's fascinating how we treat supplements like harmless candy while ignoring the fact that they're pharmacologically active compounds. The regulatory gap isn't just a loophole-it's a chasm. I've reviewed clinical studies on ginkgo and warfarin interactions, and the pharmacokinetic data is overwhelming. The body doesn't distinguish between 'natural' and 'synthetic' molecules; it only responds to chemical structure. If you're on anticoagulants, any herb with antiplatelet activity is a potential time bomb. The real issue isn't supplements-it's the cultural delusion that nature = safe. That's a dangerous oversimplification.
Kristin Jarecki
February 14, 2026 AT 15:17As a healthcare professional, I cannot emphasize enough the importance of full disclosure. In my practice, I have witnessed patients suffer adverse events-some life-threatening-because they assumed their physician didn't need to know about their herbal regimen. The TGA and FDA may not regulate supplements as drugs, but that does not mean they lack pharmacological activity. I routinely ask patients: 'What are you taking to support your health?' rather than 'Are you on any supplements?' The difference in response rate is dramatic. Honesty isn't optional-it's foundational to safe care.
Jonathan Noe
February 15, 2026 AT 09:57Let’s be real-this whole 'natural means safe' thing is pure nonsense. I used to take St. John’s wort for my anxiety because it was 'all-natural.' Then I got put on Zoloft and nearly ended up in the ER with serotonin syndrome. My doctor had no idea I was still taking it. That’s not my fault-it’s the system’s. No one warns you. No one asks. And then you’re the idiot who 'didn’t read the label.' Meanwhile, Big Pharma is making billions while herbal companies get a free pass. The FDA should treat these like drugs. Period. End of story.
Jim Johnson
February 17, 2026 AT 07:21Y’all need to chill a little. I’ve been taking fish oil, magnesium, and vitamin D for years. Never had a problem. My doc doesn’t even ask, and I’m fine. Look, I get it-some stuff can interact. But most people are fine. You don’t need to turn every supplement into a medical emergency. I mean, come on. People get mad at coffee for raising BP, but no one’s banning it. Why is this different? Just be smart. Don’t mix random stuff. Talk to your pharmacist. Done. No need for the doom-and-gloom.
Pat Mun
February 18, 2026 AT 01:11I’ve been on blood pressure meds for 8 years. I started taking turmeric extract because I read it reduces inflammation. I didn’t tell my doctor because I thought, 'It’s just a spice.' Then one day I got dizzy, almost passed out, and my BP dropped to 85/50. Turns out, curcumin potentiates antihypertensives. My doctor said, 'This happens more than you think.' Now I keep a printed list in my wallet. I hand it to every provider-even the ER nurse. I also ask them: 'What should I be avoiding?' It’s not about trust. It’s about partnership. And honestly? I feel safer now. Not because I stopped supplements-but because I started being honest.
Sophia Nelson
February 18, 2026 AT 16:34This article is fearmongering. You’re scaring people out of perfectly safe, traditional remedies because Big Pharma wants you dependent on their overpriced pills. St. John’s wort works better than SSRIs for mild depression. Ginkgo improves cognition. Green tea extract is antioxidant-rich. The real danger is the medical establishment ignoring holistic health because they’re paid per procedure, not per wellness. And don’t even get me started on how the TGA and FDA are corrupted by industry lobbying. You’re not protecting us-you’re protecting profits. I take 12 supplements. I’m healthier than 90% of people on prescriptions. So go ahead. Keep your 'evidence-based' nonsense.
Neha Motiwala
February 19, 2026 AT 22:57Ojus Save
February 21, 2026 AT 18:24Jack Havard
February 23, 2026 AT 14:47Let’s not pretend this is about safety. It’s about control. The medical-industrial complex needs you dependent on regulated, patentable substances so they can bill insurance and collect data. Supplements? They’re untraceable. Unprofitable. Uncontrollable. So now they’re painted as dangerous. The same people who sell you opioids for a headache are now telling you not to take garlic. Coincidence? I think not. If you really cared about safety, you’d regulate the damn thing. Instead, you blame the consumer. Classic.
Gloria Ricky
February 25, 2026 AT 00:32My grandma took garlic pills for 30 years and never had a stroke. My cousin took St. John’s wort and got off antidepressants. I’m not saying everyone’s fine-but blanket warnings scare people away from things that actually help. I’ve seen real healing with supplements. The problem isn’t the supplements-it’s that doctors aren’t trained to use them wisely. We need integrative medicine, not fear. Ask me what I’m taking? I’ll tell you. But don’t tell me to stop because you don’t understand it.
Stacie Willhite
February 25, 2026 AT 12:34I used to be the person who never mentioned supplements. I thought, 'It’s just a multivitamin.' Then I had a panic attack after starting a new magnesium supplement. Turns out, I was deficient in B6, and the magnesium was throwing off my neurotransmitter balance. My therapist helped me connect the dots. Now I keep a journal: what I take, when, how I feel. I bring it to every appointment. My doctor says I’m one of the most helpful patients she has. It’s not about being perfect. It’s about being aware. And yes-I still take supplements. Just now, I know why, how, and what to watch for.
Sonja Stoces
February 26, 2026 AT 00:32Gabriella Adams
February 27, 2026 AT 23:56There’s a beautiful irony here: the very people who champion natural living are often the ones most resistant to evidence-based dialogue. We can honor traditional remedies while still demanding rigorous safety standards. The goal isn’t to eliminate supplements-it’s to elevate the conversation. I’ve worked with patients who reversed prediabetes with berberine and lifestyle changes. But they also told me exactly what they took, how much, and where they bought it. We tracked their labs weekly. That’s integrative care. That’s partnership. Not fear. Not dogma. Just clarity. If your doctor dismisses you, find one who listens. And if you’re buying supplements online without third-party verification? You’re playing Russian roulette with your liver.