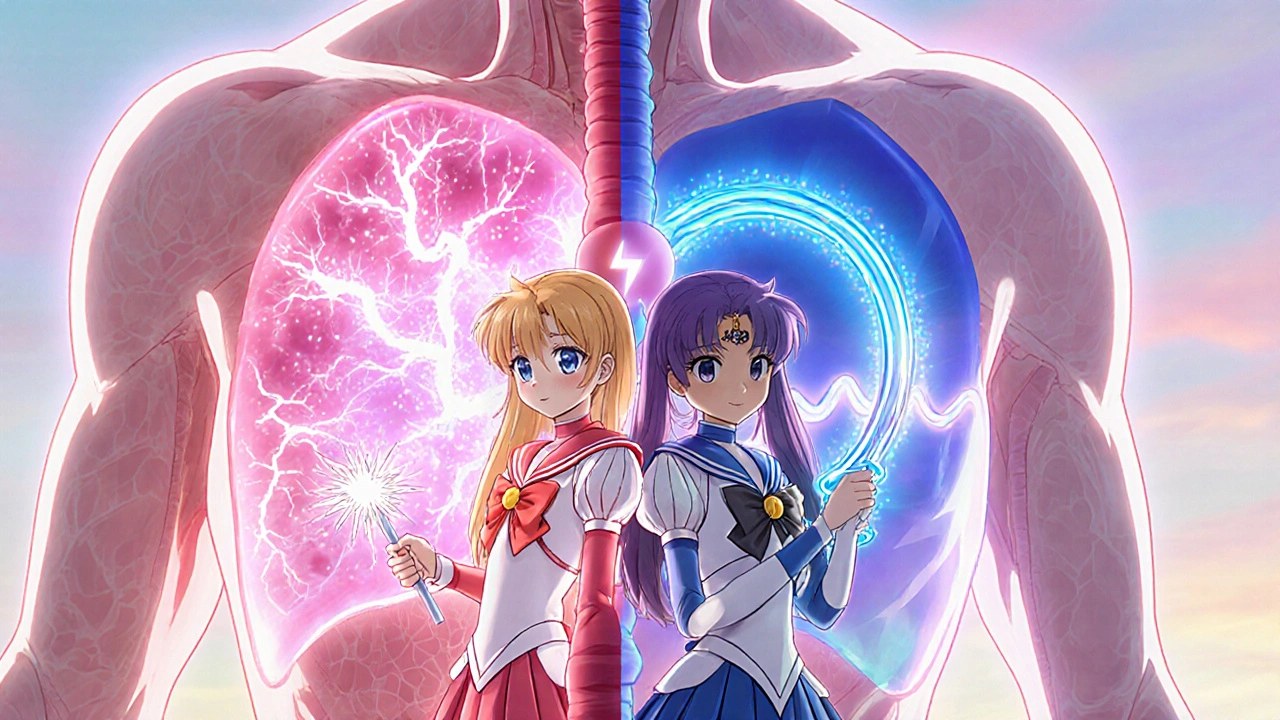
atrial fibrillation – what you need to know
When dealing with atrial fibrillation, a common heart rhythm disorder where the upper chambers beat irregularly. Also known as AF, it raises the chance of blood clots and stroke. One of the biggest worries is stroke risk, the probability of a cerebrovascular event caused by clots formed during AF. To keep that risk low, doctors often prescribe anticoagulant therapy, medications that thin the blood and prevent clot formation. At the same time, beta‑blockers, drugs that slow the heart rate and reduce strain on the heart are a mainstay for rate control. Together, these strategies aim to keep the heart beating in a safer rhythm while protecting the brain.
Why stroke risk drives treatment decisions
Every time the atria flutter, tiny clots can form and travel to the brain. Studies show that untreated AF can triple the chance of a disabling stroke. That’s why stroke risk is the first item on any doctor’s checklist. Anticoagulant therapy—whether it’s a warfarin regimen or a newer direct oral anticoagulant—cuts that risk by up to 70 percent. The choice of drug depends on kidney function, age, and potential drug interactions, but the goal stays the same: stop clots before they cause damage.
Beyond blood thinners, heart‑rate control matters just as much. If the ventricles fire too fast, the heart can’t fill properly, leading to fatigue, shortness of breath, and eventually heart failure. Beta‑blockers, calcium‑channel blockers, and certain anti‑arrhythmic pills each target the rate from a different angle. Many patients start with a beta‑blocker because it’s easy to dose, works quickly, and has a long safety record. For those who can’t tolerate beta‑blockers, doctors might switch to a non‑dihydropyridine calcium‑channel blocker like diltiazem.
When medication isn’t enough, rhythm‑control strategies come into play. Electrical cardioversion can reset the heart’s rhythm in a single session, while catheter ablation—a minimally invasive procedure that isolates problematic electrical pathways—offers a more permanent fix for many. Both approaches require a clean ECG baseline and often a short stay in a monitored setting. The decision to pursue rhythm control versus rate control hinges on symptom severity, age, and the presence of other heart diseases.
All of these options—stroke prevention, rate‑control meds, rhythm‑control procedures—are linked by a common aim: keep the heart beating smoothly and protect the brain. Below you’ll find articles that dive deeper into each of these pillars, from how to choose the right anticoagulant to the pros and cons of beta‑blocker therapy and what to expect from ablation. Use them as a roadmap to understand your condition, ask informed questions, and work with your healthcare team on a personalized plan.
Atrial Fibrillation vs Atrial Flutter: Key Differences, Symptoms & Treatment
Learn the key differences between atrial fibrillation and atrial flutter, their symptoms, risk factors, diagnosis, and treatment options in a clear, practical guide.
October 23 2025